Superior Waitlist and Equivalent Transplant Outcomes Among Hepatitis C RNA-Positive Patients Who Are Willing to Accept Hepatitis C Seropositive Kidneys.
1Surgery, University of California-Davis, Sacramento, CA
2Internal Medicine, University of California-Davis, Sacramento, CA.
Meeting: 2016 American Transplant Congress
Abstract number: 218
Keywords: Donors, Hepatitis C, Kidney transplantation, marginal, Waiting lists
Session Information
Session Name: Concurrent Session: Kidney Transplantation: Allocation, Discard, and HCV
Session Type: Concurrent Session
Date: Monday, June 13, 2016
Session Time: 2:30pm-4:00pm
 Presentation Time: 3:30pm-3:42pm
Presentation Time: 3:30pm-3:42pm
Location: Veterans Auditorium
Background: kidney transplantation from hepatitis C seropositive (HCV+) donors may benefit hepatitis C RNA-positive (RNA+) candidates, but it is not clear how the acceptance/listing status of such kidneys affect waitlist and transplant outcomes.
Methods: In a single-center retrospective analysis, HCV+ transplant candidates (N=169) who were placed on the deceased donor kidney waitlist from March 2004 to February 2015 were evaluated for waitlist and posttransplant outcomes. All RNA+ candidates were offered the option to be listed for HCV+ donors (in addition to HCV seronegative [HCV-] donors) in UNet after informed consent was obtained. RNA- candidates were listed only for HCV- donors.
Results: Fifty-seven patients (51% of all RNA+) were willing to accept HCV+ kidneys and listed both for HCV+ and HCV- donors. During 6-yr follow up, 43 of 57 (75%) RNA+ patients accepting HCV+ donors vs. 19 of 55 (35%) RNA+ patients not accepting HCV+ donors received a deceased donor kidney transplant with median waiting time of 9 mo vs. 45 mo, respectively (P<0.0001). 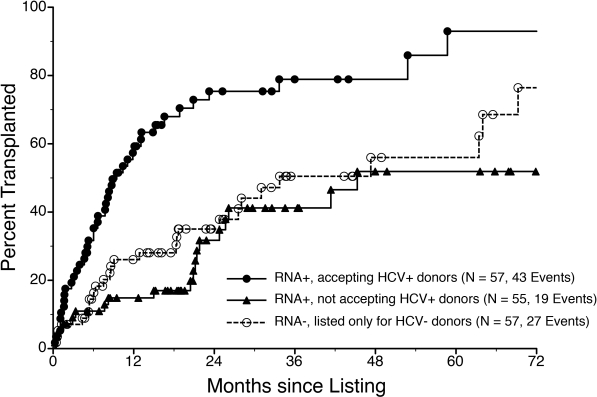 Multivariable analysis demonstrated that HCV listing status (P=0.0005) and waiting time (P<0.0001) were associated with receiving a transplant. More patients not accepting HCV+ donors (vs. accepting HCV+ donors) were removed from the list due to death or deteriorated medical condition (20% vs. 4%, P=0.0046). Posttransplant patient survival rates were similar for patients accepting vs. not accepting HCV+ donors (70% vs. 67% at 6 yrs, P=0.55). On multivariable analysis, donor HCV status did not impact posttransplant patient or graft survival. Patient and graft survival rates for HCV+ vs. HCV- donor transplants at 6 yrs were 74% vs. 59% (P=0.93) and 59% vs. 52% (P=0.43), respectively.
Multivariable analysis demonstrated that HCV listing status (P=0.0005) and waiting time (P<0.0001) were associated with receiving a transplant. More patients not accepting HCV+ donors (vs. accepting HCV+ donors) were removed from the list due to death or deteriorated medical condition (20% vs. 4%, P=0.0046). Posttransplant patient survival rates were similar for patients accepting vs. not accepting HCV+ donors (70% vs. 67% at 6 yrs, P=0.55). On multivariable analysis, donor HCV status did not impact posttransplant patient or graft survival. Patient and graft survival rates for HCV+ vs. HCV- donor transplants at 6 yrs were 74% vs. 59% (P=0.93) and 59% vs. 52% (P=0.43), respectively.
Conclusion: HCV RNA+ patients significantly benefit if they are willing to accept HCV+ kidneys as they have superior waitlist and equivalent transplant outcomes.
CITATION INFORMATION: Sageshima J, de Mattos A, Troppmann C, Santhanakrishnan C, McVicar J, Gallay B, Gandhi M, Alnimri M, Perez R. Superior Waitlist and Equivalent Transplant Outcomes Among Hepatitis C RNA-Positive Patients Who Are Willing to Accept Hepatitis C Seropositive Kidneys. Am J Transplant. 2016;16 (suppl 3).
To cite this abstract in AMA style:
Sageshima J, Mattos Ade, Troppmann C, Santhanakrishnan C, McVicar J, Gallay B, Gandhi M, Alnimri M, Perez R. Superior Waitlist and Equivalent Transplant Outcomes Among Hepatitis C RNA-Positive Patients Who Are Willing to Accept Hepatitis C Seropositive Kidneys. [abstract]. Am J Transplant. 2016; 16 (suppl 3). https://atcmeetingabstracts.com/abstract/superior-waitlist-and-equivalent-transplant-outcomes-among-hepatitis-c-rna-positive-patients-who-are-willing-to-accept-hepatitis-c-seropositive-kidneys/. Accessed February 27, 2026.« Back to 2016 American Transplant Congress
