Incidence and Renal Consequences of Type 2 Diabetes Mellitus in Kidney Donors.
U of MN, Mpls.
Meeting: 2016 American Transplant Congress
Abstract number: 50
Session Information
Session Name: Concurrent Session: Living Kidney Donation: Risk Factors for Adverse Long term Outcome
Session Type: Concurrent Session
Date: Sunday, June 12, 2016
Session Time: 2:30pm-4:00pm
 Presentation Time: 2:54pm-3:06pm
Presentation Time: 2:54pm-3:06pm
Location: Veterans Auditorium
Diabetes Mellitus (DM) continues to be the most common cause of kidney disease. The incidence of DM following kidney donation is unknown. Moreover, whether its development in someone who donated a kidney in the past results in accelerated GFR change, compared to non-diabetic donors and those with 2 kidneys, has not been studied.
We determined the incidence and predictors of DM development in 3956 White kidney donors who donated between 1963-2013 and performed a case control study of 208 donors who developed DM and 208 without DM after matching on age, gender, BMI, eGFR and glucose at donation and year of donation. The main outcomes of interest for the matched analysis were hypertension development, proteinuria and reduced GFR.
After a mean follow-up of 16.6±11.9 yrs, 231 (6.7%) donors developed diabetes requiring treatment at a median age of 56.6 years. After adjusting for age, gender, BMI and glucose at donation and year of donation, pre-donation risk factors for DM included: body mass index; HR 1.13 (95% CI 1.11-1.16), p<0.0001; fasting glucose; HR 1.01 (95% CI 1.01-1.02), p<0.0001; and history of smoking; HR 1.51 (95% CI 1.15-1.98), p<0.01. Women were less likely to develop DM; HR 0.78 (95% CI 0.6-1.0), p=0.05.
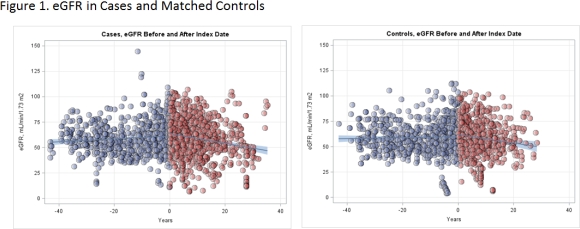
In the matched analysis, diabetic donors were more likely to become hypertensive (71% vs 43%) and proteinuric (26% vs 11%). Annual eGFR change after DM development was -0.48 ml/min/1.73m2 (95% CI -0.62,-0.34) in cases and -0.42 ml/min/1.73m2 (95% CI -0.66, -0.80) in controls. These rates are almost identical to the rates reported in the INDT trial which studied microalbuminuric hypertensive type 2 diabetic individuals. When DM was considered as a conditional time-dependent covariate, it was modestly associated with reaching an eGFR < 60 ml/in/1.73m2; HR 1.26 (95% CI 0.99-1.61), p=.06 or an eGFR < 30; HR 1.69 (95% CI 0.97-2.69), p=0.06 but not ESRD; HR 2.42 (95% CI 0.82-7.1), p=0.10.
Incidence and risk factors of DM in kidney donors are similar to what is seen in the general population. Kidney donors who develop diabetes, compared to non-diabetic donors, after donation are more likely to be hypertensive, proteinuric, have a slightly higher risk of reduced GFR but not ESRD.
CITATION INFORMATION: Ibrahim H, Matas A, Berglund D, Reule S, Kukla A, Issa N, Spong R, Foley R. Incidence and Renal Consequences of Type 2 Diabetes Mellitus in Kidney Donors. Am J Transplant. 2016;16 (suppl 3).
To cite this abstract in AMA style:
Ibrahim H, Matas A, Berglund D, Reule S, Kukla A, Issa N, Spong R, Foley R. Incidence and Renal Consequences of Type 2 Diabetes Mellitus in Kidney Donors. [abstract]. Am J Transplant. 2016; 16 (suppl 3). https://atcmeetingabstracts.com/abstract/incidence-and-renal-consequences-of-type-2-diabetes-mellitus-in-kidney-donors/. Accessed February 11, 2026.« Back to 2016 American Transplant Congress
