Surgical Complication Rates in Patients Receiving Kidney Transplants in England: Analysis by Transplant Centre Using Linked Registry and Hospitalisation Data
Sheffield Kidney Institute, Northern General Hospital, Sheffield, South Yorkshire, United Kingdom
School of Health and Related Research, University of Sheffield, Sheffield, South Yorkshire, United Kingdom
Meeting: 2013 American Transplant Congress
Abstract number: D1739
Introduction: Previous UK studies have found similar centre-specific graft and patient survival following first transplantation, however other measures of surgical performance have not previously been reported at a national level.
Methods: First transplants (T1) in patients starting renal replacement therapy between 2002 and 2006 were identified in UK Renal Registry data linked with Hospital Episode Statistics (HES) data. Surgical complications out to 12 months and comorbidity at T1 were identified using HES diagnosis and procedure codes. Standardised complication rate ratios were determined using observed/expected counts predicted using logistic regression.
Results: 4,517 T1 were identified in both sources in 20 centres. Surgical complication rates were: any complication 22.3%, ureteric 7%, vascular 3.1%, wound 5.3%, venous thrombosis 1.3%, complication requiring exploration and nephrectomy 5.1% and 3.9% respectively, misc 4.8%. Deceased donor (DD) recipients and diabetics had higher surgical complication rates (27.2% vs 21.1%, P<0.001, and 23.7% vs 19.5%, P=0.002). Wound complications were higher in peritoneal dialysis than haemodialysis or pre-emptively transplanted patients (6.7% vs 4.9% and 3.1% respectively, P=0.002). Ureteric complications were similar in patients with and without ureteric stents (6.5% vs 7.5%, P=0.198). Delayed graft failure (DGF) was 17.6% in DD, 3.6% in live donor and DGF was associated with a higher incidence of surgical complication (20.2% vs 36.4%, P<0.001). Following adjustment for age, diabetes, donor type and centre coding depth the number of centres with higher than expected surgical complications was increased from 4 to 5, with better than expected centres reduced from 4 to 1.
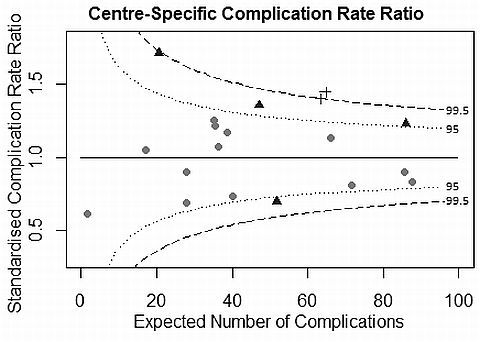
Conclusions: Routine linked data can enable the reporting of surgical complications and DGF at a national level. Following adjustment, outlying centres persist. Consistent HES coding practice would strengthen future studies.
To cite this abstract in AMA style:
Fotheringham J, Campbell M, El-Nahas M, Shretha B, McKane W. Surgical Complication Rates in Patients Receiving Kidney Transplants in England: Analysis by Transplant Centre Using Linked Registry and Hospitalisation Data [abstract]. Am J Transplant. 2013; 13 (suppl 5). https://atcmeetingabstracts.com/abstract/surgical-complication-rates-in-patients-receiving-kidney-transplants-in-england-analysis-by-transplant-centre-using-linked-registry-and-hospitalisation-data/. Accessed February 16, 2026.« Back to 2013 American Transplant Congress
