Decision-Making Among HCV-Negative Transplant Candidates Offered Organs from Donors with HCV Infection
E. Schnellinger1, E. Saine1, M. Liu1, J. Diamond1, M. Crespo1, S. Prenner1, V. Potluri1, C. Bermudez1, H. Mentch1, M. Moore2, B. Besharatian1, D. Goldberg3, F. Barg1, P. Reese1
1University of Pennsylvania, Philadelphia, PA, 2University of London, London, United Kingdom, 3University of Miami, Miami, FL
Meeting: 2022 American Transplant Congress
Abstract number: 555
Keywords: Hepatitis C, Informed consent, Organ Selection/Allocation, Psychosocial
Topic: Clinical Science » Infection Disease » 27 - Non-Organ Specific: Viral Hepatitis
Session Information
Session Time: 5:30pm-7:00pm
 Presentation Time: 5:50pm-6:00pm
Presentation Time: 5:50pm-6:00pm
Location: Hynes Room 312
*Purpose: Historically, many organs from deceased donors with hepatitis C virus (HCV) infection were discarded due to stigma and challenges in treating HCV after transplant. The advent of direct acting antiviral therapies led transplant centers to conduct trials of transplanting HCV-RNA+ donor organs into HCV-negative recipients, followed by antiviral therapy. However, factors that influence candidates’ decisions to accept or decline transplant with HCV-RNA+ organs are not well understood.
*Methods: To explore patient-level perceptions, influences, and experiences that inform decision-making regarding transplant with HCV-RNA+ donor organs, we conducted a qualitative semi-structured interview study embedded within three clinical trials involving transplantation of lungs or kidneys from HCV-RNA+ donors into HCV-negative recipients. The study was conducted June 2019 – March 2021.
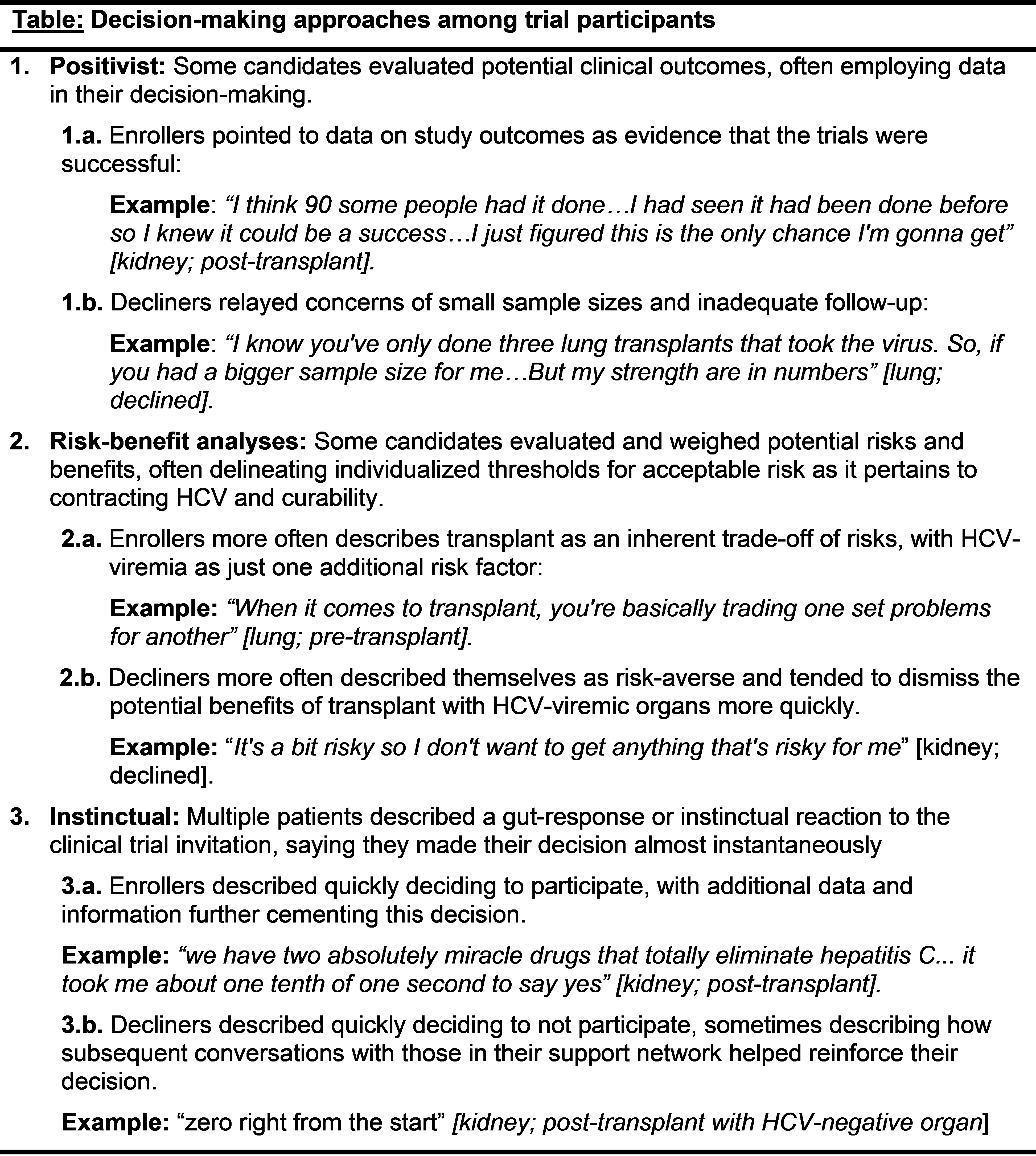
*Results: Forty-four HCV-negative waitlisted patients participated in the qualitative study, among whom 33 enrolled in a trial and 11 declined to join a trial. Participants had diverse ways of thinking about risk and that diversity contributed to how they made decisions. Three approaches to decision-making about HCV-RNA transplant emerged: positivist (meaning that decisions must be backed up by scientific/experimental evidence), risk-benefit analyses, and instinctual response. The Table presents quotes that exemplify these three approaches to decisions. Moreover, most participants relied on multiple decision-making approaches either simultaneously or sequentially.
*Conclusions: A better understanding of how different decisional models influence patients’ decisions about transplant with organs from HCV-infected donors may promote shared decision-making among transplant patients and providers. These detailed findings may also be applicable to decision-making with other types of higher-risk organs.
To cite this abstract in AMA style:
Schnellinger E, Saine E, Liu M, Diamond J, Crespo M, Prenner S, Potluri V, Bermudez C, Mentch H, Moore M, Besharatian B, Goldberg D, Barg F, Reese P. Decision-Making Among HCV-Negative Transplant Candidates Offered Organs from Donors with HCV Infection [abstract]. Am J Transplant. 2022; 22 (suppl 3). https://atcmeetingabstracts.com/abstract/decision-making-among-hcv-negative-transplant-candidates-offered-organs-from-donors-with-hcv-infection/. Accessed March 7, 2026.« Back to 2022 American Transplant Congress