DCD vs DBD Pancreas Transplant Outcome – A Comprehensive Registry Analysis
1SUNY Downstate Medical Center, Brooklyn, NY, 2Medicine, SUNY Downstate Medical Center, Brooklyn, NY
Meeting: 2022 American Transplant Congress
Abstract number: 428
Keywords: Donors, non-heart-beating, Pancreas transplantation, Risk factors
Topic: Clinical Science » Pancreas » 65 - Pancreas and Islet: All Topics
Session Information
Session Name: Pancreas and Islet: All Topics
Session Type: Rapid Fire Oral Abstract
Date: Tuesday, June 7, 2022
Session Time: 3:30pm-5:00pm
 Presentation Time: 3:40pm-3:50pm
Presentation Time: 3:40pm-3:50pm
Location: Hynes Room 210
*Purpose: Pancreas transplantation offers long-term independence from insulin injections for patients with labile diabetes mellitus. After a decade of decline (2004-2015), the number of pancreas transplants has finally increased again, particularly in the simultaneous pancreas and kidney (SPK) category due to excellent outcome. However, the number of suitable donor pancreata is limited primarily because of donor age limitations and organ quality. Hence, pancreata with extended donor criteria are rarely considered for transplantation. The purpose of this study was to compare transplant outcome between donation after cardiac death (DCD) vs donation after brain death (DBD).
*Methods: All primary simultaneous pancreas/kidney (SPK) transplants between 1/1/2011 and 12/31/2020 were included. Comprehensive descriptive analyses of patient, donor, and transplant characteristics were performed as well as analysis of follow-up status. Patient and graft survival was assessed using the Kaplan-Meier method. A risk assessment model was developed using Cox regression.
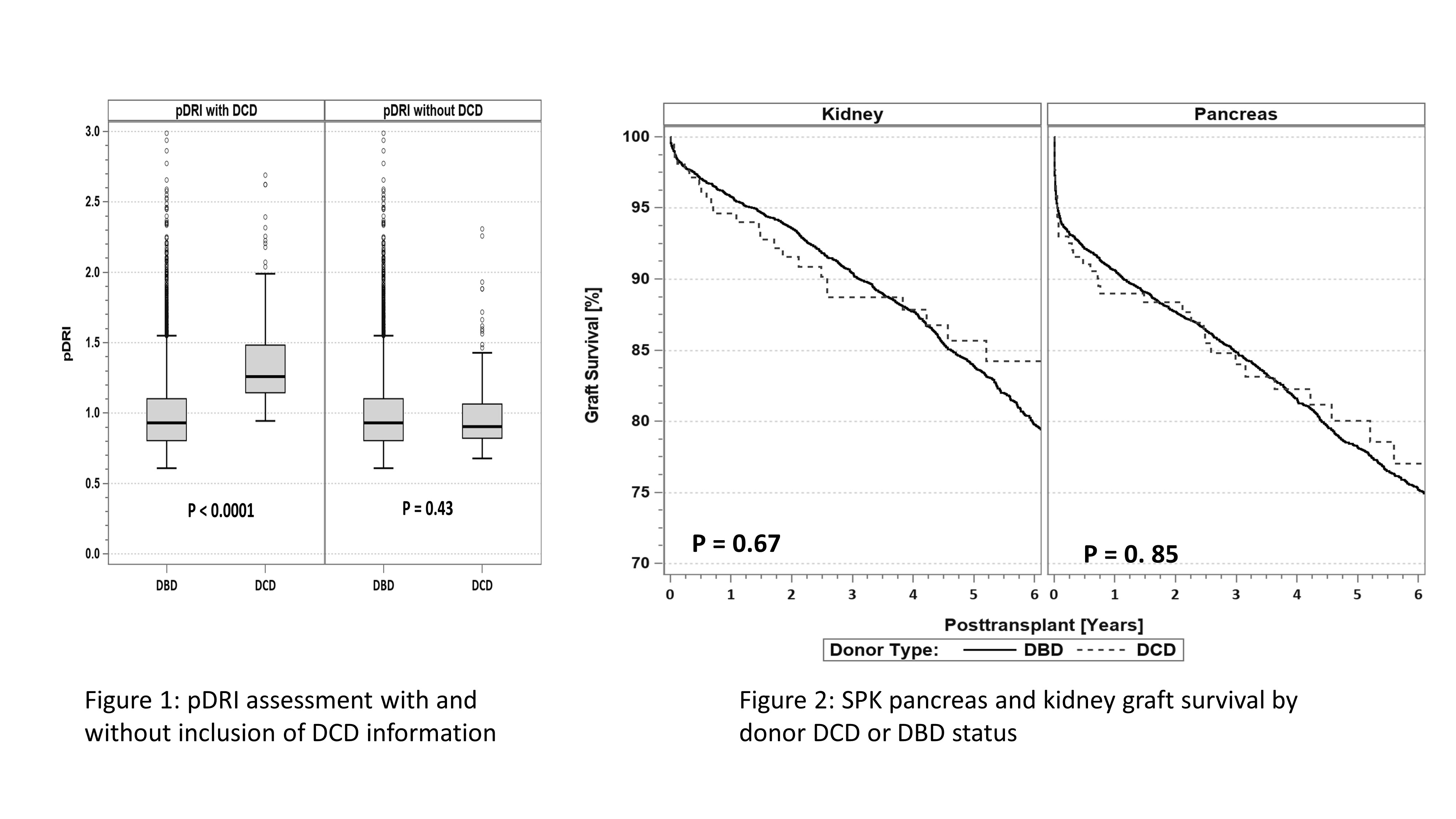
*Results: Out of 7,621 primary SPK transplants only 3% came from DCD donors. DCD donors were on average younger than DBD donors, and more often White. pDRI was significantly higher in DCD donors but removing the DCD factor from the formula revealed no differences (Figure 1). Significantly more high-volume centers accepted DCD pancreas donors. The same finding was noted for the kDPI. SPK patient and graft survival was comparable between DCD and DBD donors and was excellent in both groups (Figure 2). The only difference was noted in DCD kidneys with a significantly higher delayed graft function rate: 23% for DCD vs 7.4% for DBD (p<0.0001). Of note, the delayed graft function rate was significantly lower for DCD kidney grafts shipped on pump (p< 0.05) but was still significantly higher compared to DBD kidneys. A multivariable risk analysis for pancreas and kidney graft survival identified only donor and recipient age, recipient BMI, and center volume, but not DCD donor type, as risk factors.
*Conclusions: Due to high organ quality standards, a pancreas graft is less often accepted for transplantation than a kidney graft. Our analysis showed that outcome of pancreas transplants from DCD donors are equivalent to DBD donors. We also noted that donor management advancements such as normo- or hypothermic perfusion, persufflation of both pancreas and kidney significantly widen the donor pool and improve DCD transplant outcome.
To cite this abstract in AMA style:
Gruessner AC, Saggi SJ, Gruessner R. DCD vs DBD Pancreas Transplant Outcome – A Comprehensive Registry Analysis [abstract]. Am J Transplant. 2022; 22 (suppl 3). https://atcmeetingabstracts.com/abstract/dcd-vs-dbd-pancreas-transplant-outcome-a-comprehensive-registry-analysis/. Accessed February 17, 2026.« Back to 2022 American Transplant Congress