Is Abo Incompatible Living Donor Liver Transplantation Really a Good Alternative for Pediatric Recipients?
1Pediatric Surgery and Transplantation Unit, Cliniques Universitaires St Luc, Brussels, Belgium, 2Pediatric Gastroenterology And Hepatology division, Cliniques Universitaires St Luc, Brussels, Belgium, 3Pathology department, Cliniques Universitaires St Luc, Brussels, Belgium, 4Institute of Experimental and Clinical Research, Université Catholique de Louvain, Brussels, Belgium, 5Laboratoire Hospitalier Universitaire de Bruxelles, Université Libre de Bruxelles, Brussels, Belgium
Meeting: 2022 American Transplant Congress
Abstract number: 326
Keywords: Kidney/liver transplantation, Living donor, Pediatric
Topic: Clinical Science » Liver » 61 - Liver: Pediatrics
Session Information
Session Time: 5:30pm-7:00pm
 Presentation Time: 5:50pm-6:00pm
Presentation Time: 5:50pm-6:00pm
Location: Hynes Room 311
*Purpose: ABO incompatible (ABOi) living donor liver transplantation (LDLT) has been proposed to compensate for donor shortage. To date, few studies have reported detailed ABOi LDLT results in large series of pediatric patients. C4d complement deposition in graft capillaries has been reported to be associated with antibody-mediated rejection in kidney and other solid organ transplantations.
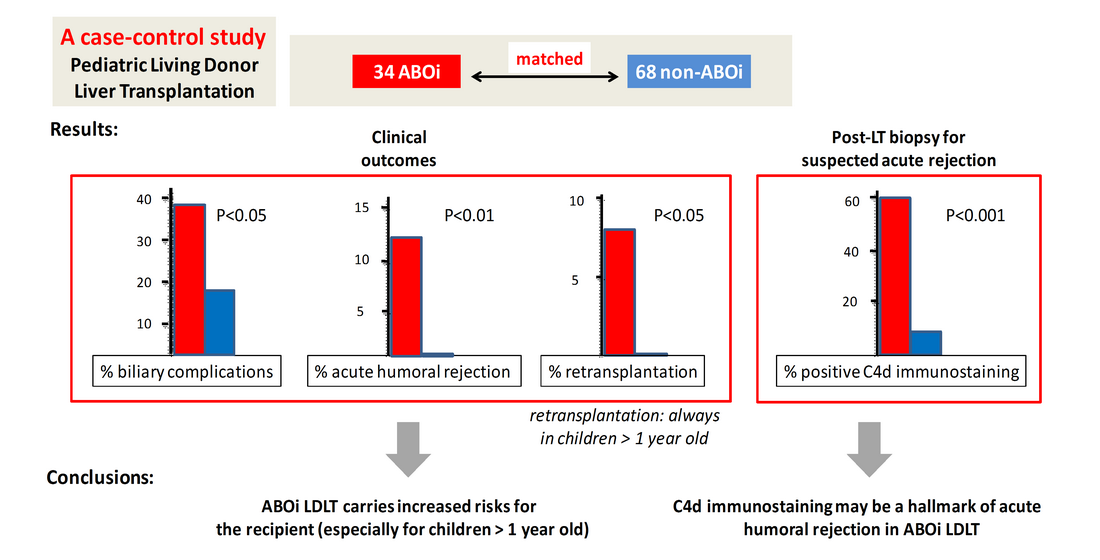
*Methods: A retrospective case-control study was conducted comparing clinical outcomes of each of 34 consecutive pediatric ABOi LDLT recipients with those from two non-ABOi pairs (n=68). A specific immunosuppresive protocol was applied to ABOi recipients based on their pre- and post-transplant iso-agglutinins titers. In addition, we studied the C4d immunostaining pattern in 22 ABOi and in 36 non-ABOi recipients whose liver biopsy was performed within the first 4 post-transplant weeks for suspected acute rejection.
*Results: The incidence of biliary complications was higher in ABOi recipients (p<0.05), as was the incidence of acute humoral rejection (p<0.01), and the incidence of retransplantation (p<0.05). All children who required a retransplantation were older than 1 year at the time of ABOi LDLT. The indication for retransplantation was diffuse intrahepatic bile duct injuries in all cases, an entity that always occurred within the first 4 months after ABOi liver transplantation. Positive C4d immunostainng was observed on the post-transplant liver graft biopsy of 13/22 (59%) ABOi recipients, versus 3/36 (8.3%) non-ABOi recipients (p<0.0001). All ABOi recipients who required a retransplantation have had a positive C4d immunostaining on their liver graft biopsy.
*Conclusions: ABOi LDLT is a feasible option for pediatric end-stage liver disease, but carries increased risks for the recipient, especially for children older than 1 year, even with a specific preparation protocol. C4d immunostaining may be a hallmark of acute humoral rejection in ABOi liver transplantation.
To cite this abstract in AMA style:
Magnée Cde, Brunée L, Tambucci R, Pire A, Scheers I, Sokal E, Baldin P, Zech F, Eeckhoudt S, Reding R, Stephenne X. Is Abo Incompatible Living Donor Liver Transplantation Really a Good Alternative for Pediatric Recipients? [abstract]. Am J Transplant. 2022; 22 (suppl 3). https://atcmeetingabstracts.com/abstract/is-abo-incompatible-living-donor-liver-transplantation-really-a-good-alternative-for-pediatric-recipients/. Accessed March 7, 2026.« Back to 2022 American Transplant Congress