Cardiac Catheterization in ESKD Patients with High Cardiovascular Risk Prior to Kidney Transplantation
L. Morena1, A. Al Jurdi2, M. S. Bittencourt3, A. C. Bucay2, N. Elias1, R. Palsson2, L. V. Riella1
1Transplant Surgery, Massachusetts General Hospital - Harvard Medical School, Boston, MA, 2Transplant Nephrology, Massachusetts General Hospital - Harvard Medical School, Boston, MA, 3Cardiac Imaging, Cardiology, University of Pittsburgh, Pittsburgh, PA
Meeting: 2022 American Transplant Congress
Abstract number: 27
Keywords: Kidney, Kidney transplantation, Post-operative complications, Survival
Topic: Clinical Science » Kidney » 35 - Kidney: Cardiovascular and Metabolic Complications
Session Information
Session Name: Kidney: Cardiovascular and Metabolic Complications I
Session Type: Rapid Fire Oral Abstract
Date: Sunday, June 5, 2022
Session Time: 3:30pm-5:00pm
 Presentation Time: 4:10pm-4:20pm
Presentation Time: 4:10pm-4:20pm
Location: Hynes Veterans Auditorium
*Purpose: Cardiovascular disease is the leading cause of death after kidney transplantation (KT), with a high risk of myocardial infarction (MI) in the peri-transplantation period. Consequently, coronary catheterization (CC) has been used in high-risk KT candidates, including asymptomatic individuals, to detect obstructive coronary artery disease (CAD) and, if necessary, allow for revascularization before KT. More recently, the benefit of coronary interventions in patients with advanced CKD has been questioned. Our study characterizes outcomes of patients who underwent CC during their transplant evaluation and evaluated intervention rates/types and post-transplant cardiovascular events.
*Methods: Single-center retrospective analysis of all high-risk adult patients who underwent KT between 2016 and 2019 and had a diagnostic CC pre-operatively, with or without subsequent revascularization. High-risk patients were defined as those with a history of diabetes mellitus, CAD, left ventricular ejection fraction (LEF)<50%, or ventricular arrhythmias. The primary composite endpoint (CE) was characterized by primary arrhythmias, non-fatal MI, coronary revascularization, or death.
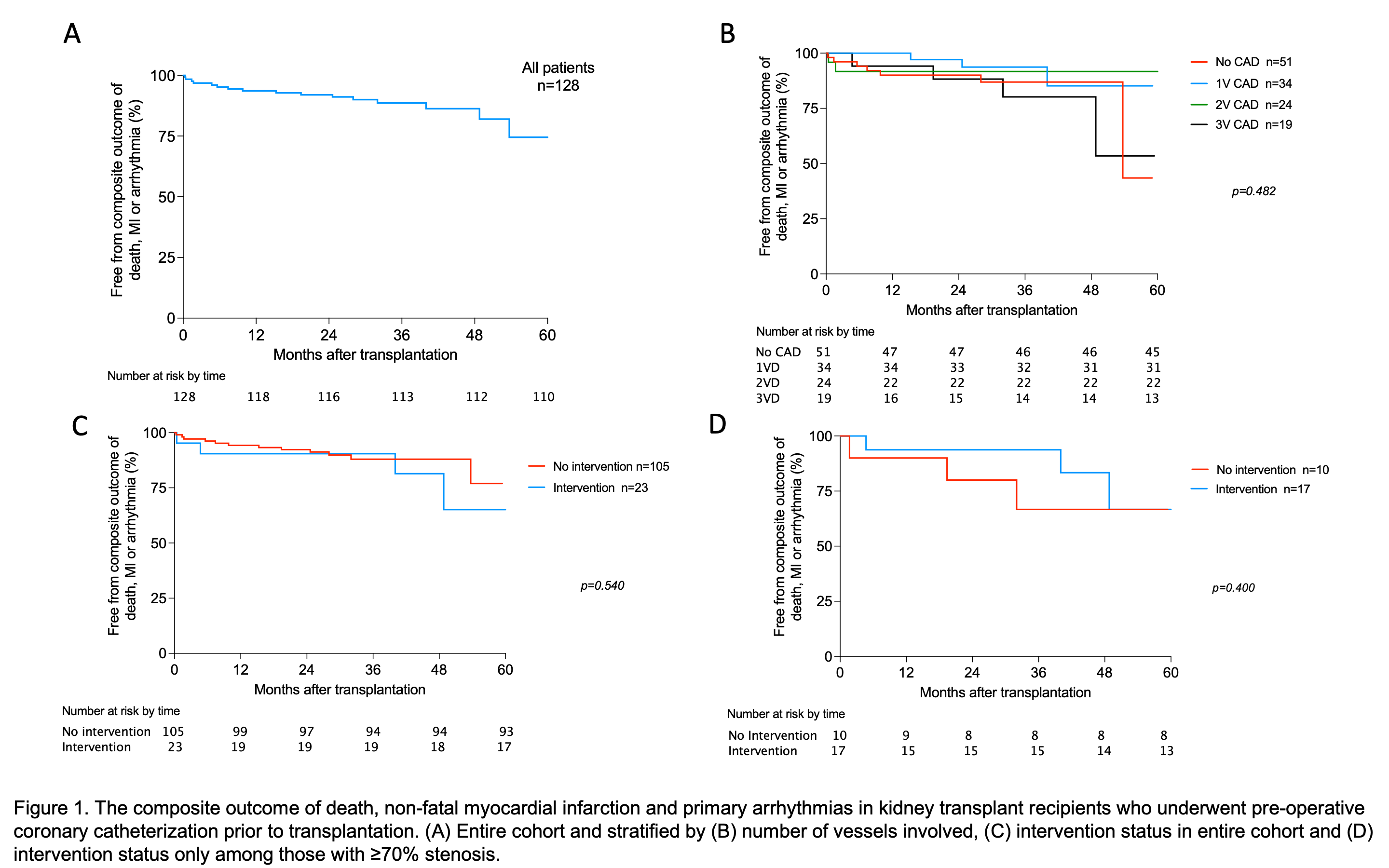
*Results: 128 patients were included. 37% were female and the mean age was 57.5±10 years. The median follow-up was 2.7 years. 23% had a significant CAD (occlusion ≥70% and/or three-vessel disease). Only 18% of the entire cohort underwent revascularization (43% stent placement, 57% CABG), which was independent of prior stress test (ST) results (P=0.319). The CE occurred in 14% of patients at two years (Figure 1A). We found no significant difference in event-free survival when stratifying by CC findings, revascularization across the entire cohort, or revascularization across those with lesions ≥70% (P values 0.593, 0.540, and 0.400, respectively, Figure 1B-D). Older age (P=0.046), LEF<50% (P=0.037), and pre-transplant CAD (P=0.042) were all associated with higher odds of CE in univariable analysis.
*Conclusions: We demonstrate a low rate of intervention after diagnostic CC in KT recipients. There was no significant difference in CE-free survival of patients when stratified by CC findings, revascularization across the entire cohort, or revascularization across those with lesions ≥70%.
To cite this abstract in AMA style:
Morena L, Jurdi AAl, Bittencourt MS, Bucay AC, Elias N, Palsson R, Riella LV. Cardiac Catheterization in ESKD Patients with High Cardiovascular Risk Prior to Kidney Transplantation [abstract]. Am J Transplant. 2022; 22 (suppl 3). https://atcmeetingabstracts.com/abstract/cardiac-catheterization-in-eskd-patients-with-high-cardiovascular-risk-prior-to-kidney-transplantation/. Accessed February 6, 2026.« Back to 2022 American Transplant Congress