Portal Vein Challenges in Pediatric Liver Transplantation: The Utility of Interposition Grafts as an Acceptable Management Strategy
Division of Hepatobiliary and Abdominal Organ Transplantation, Keck School of Medicine of USC, University of Southern California, Los Angeles, CA
Meeting: 2021 American Transplant Congress
Abstract number: 1166
Keywords: Biliary atresia, Liver grafts, Pediatric, Portal veins
Topic: Clinical Science » Liver » Liver: Pediatrics
Session Information
Session Name: Liver: Pediatrics
Session Type: Poster Abstract
Session Date & Time: None. Available on demand.
Location: Virtual
*Purpose: To examine our single center experience in the operative management of pediatric liver transplantation (LT) patients with challenging portal vein (PV) anomalies.
*Methods: We retrospectively reviewed the records of LTs performed at Children’s Hospital Los Angeles from 2004-2020. The incidence of portal vein thrombosis (PVT), atresia (PVA), and hypoplasia (PVH), operative management, and post-operative outcomes were noted. The Yerdel classification was used to classify PVT. We analyzed survival outcomes using a Kaplan-Meier estimator.
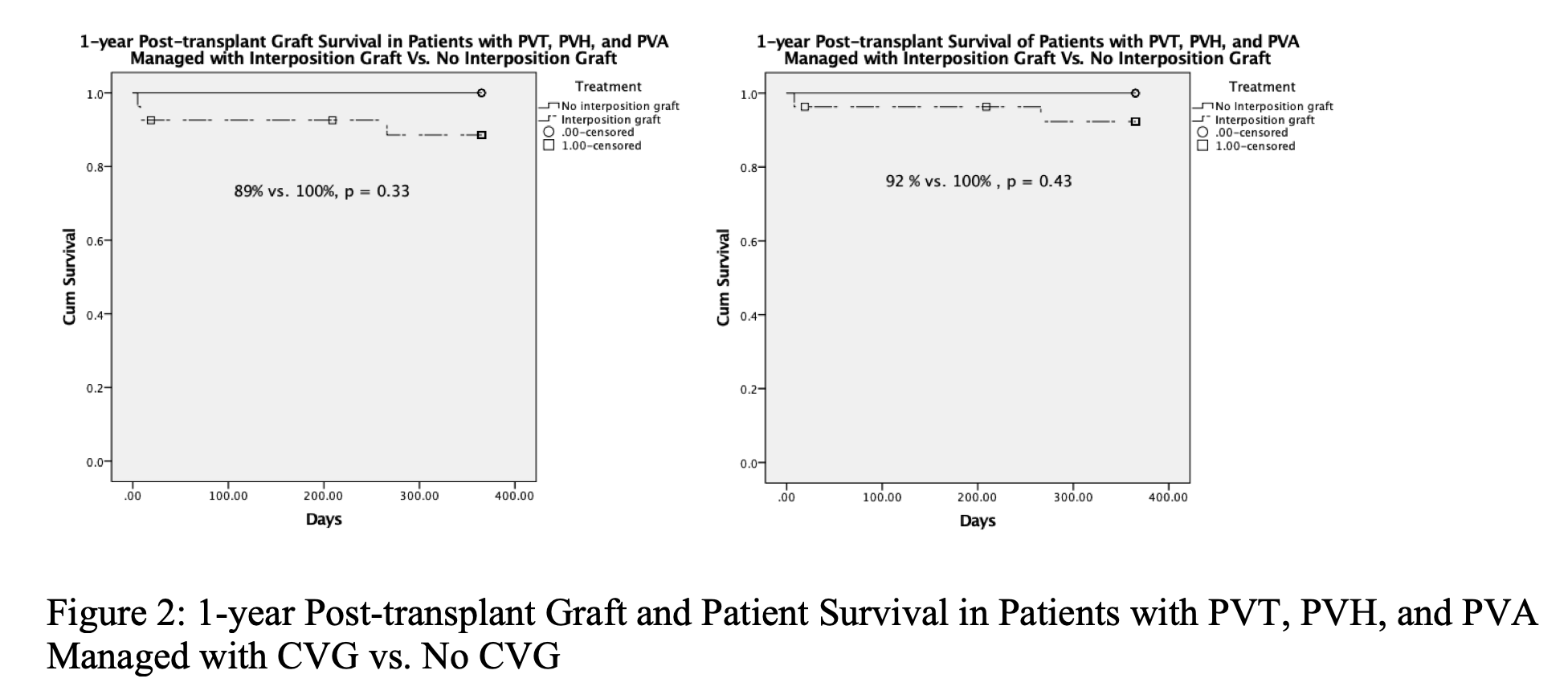
*Results: From 2004-2020, 330 pediatric LTs were performed. 22 patients (7%) had PVT (4 grade 1, 10 grade 2, 2 grade 3, 5 de-novo intra-operative, 1 unclassified), 1 (0.3%) patient had PVA, and 11 (3%) patients had PVH. The prevalence of PVT and PVH was highest in patients with BA followed by hepatoblastoma (Figure 1). 10 of 11 PVHs and one case of Abernathy malformation (PVA) were managed with a cadaveric external iliac vein interposition graft (CVG). 15 of 22 PVTs (1/4 grade 1, 8/10 grade 2, 2/2 grade 3, 3/5 de-novo) were managed with CVG. The remainder of the PVTs were managed with thrombectomy. One CVG was performed for a short PV. There was no statistically significant difference in post-operative PV complications (11% (3/27) vs. 0% (0/8); p = 1.00), re-operation for bleeding (3.7% (1/27) vs. 12.5% (1/8); p = 0.41), or LOS (30 vs. 36 days; p = 0.77) between the patients managed with CVG and those without. There were no post-operative PV complications observed in living donor grafts. Median follow up was 1381 days. There was no statistically significant difference in graft or patient survival between patients managed with CVG and those without (Figure 2).
*Conclusions: PVT, PVA, and PVH can present as challenging cases in pediatric LT. A primary construct with or without thrombectomy should be utilized when amenable. However, many circumstances arise when thrombectomy is inadequate or the native vessel itself is of critically small caliber. As we have shown, such instances can safely and successfully be managed utilizing a CVG with excellent outcomes.
To cite this abstract in AMA style:
Hogen R, Etesami K, Cervantes J, Kwon Y, Zielsdorf S, Emamaullee J, Genyk Y. Portal Vein Challenges in Pediatric Liver Transplantation: The Utility of Interposition Grafts as an Acceptable Management Strategy [abstract]. Am J Transplant. 2021; 21 (suppl 3). https://atcmeetingabstracts.com/abstract/portal-vein-challenges-in-pediatric-liver-transplantation-the-utility-of-interposition-grafts-as-an-acceptable-management-strategy/. Accessed January 23, 2026.« Back to 2021 American Transplant Congress