Comparison of Allograft Outcomes in SLK Transplant Patients with and without ESLD: A UNOS Database Analysis
Transplant Division, Beth Israel Deaconess Medical Center, Boston, MA
Meeting: 2021 American Transplant Congress
Abstract number: 1084
Keywords: Kidney/liver transplantation
Topic: Clinical Science » Liver » Liver: Kidney Issues in Liver Transplantation
Session Information
Session Name: Liver: Kidney Issues in Liver Transplantation
Session Type: Poster Abstract
Session Date & Time: None. Available on demand.
Location: Virtual
*Purpose: Simultaneous liver and kidney transplants (SLKT) have started to gain ground in the treatment of liver disease with associated acute or chronic kidney disease. In certain metabolic liver diseases with resultant kidney failure, SLKT is performed to help improve kidney graft survival, when the liver function is seemingly normal. Primary hyperoxaluria (PH), a rare autosomal recessive liver disease that leads to kidney failure and is the most common cause of metabolic liver disease treated with SLKT.
SLKT is known to provide immunological protection for kidney allograft, as compared to kidney alone, for unclear reasons. In this analysis, we compared the allograft survival in patients with and without End-Stage Liver Disease and explored whether this immune tolerance is enhanced by the presence of ESLD pre-transplant, similar to how bone marrow transplant patients undergo a preparative regimen to create an environment conducive to long-term engraftment.
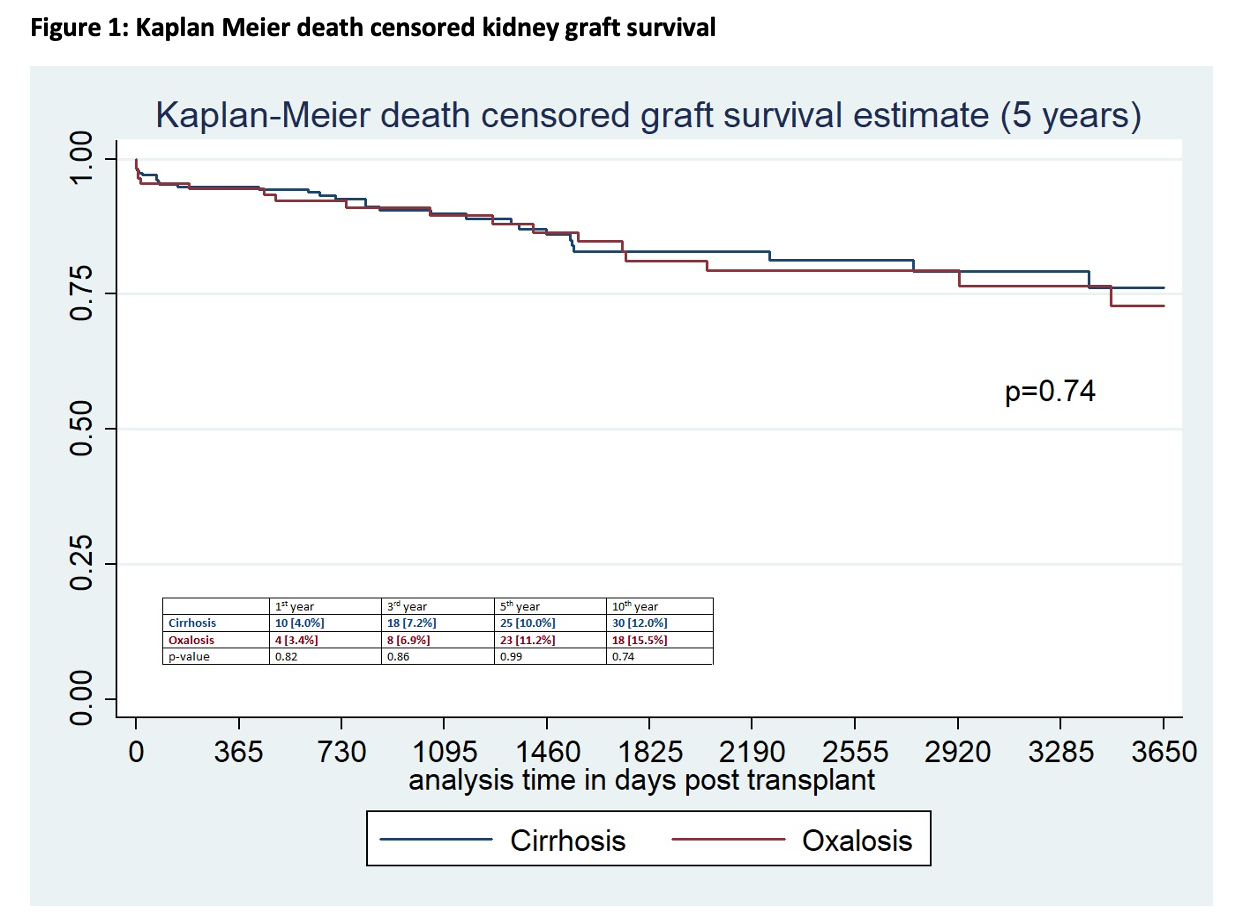
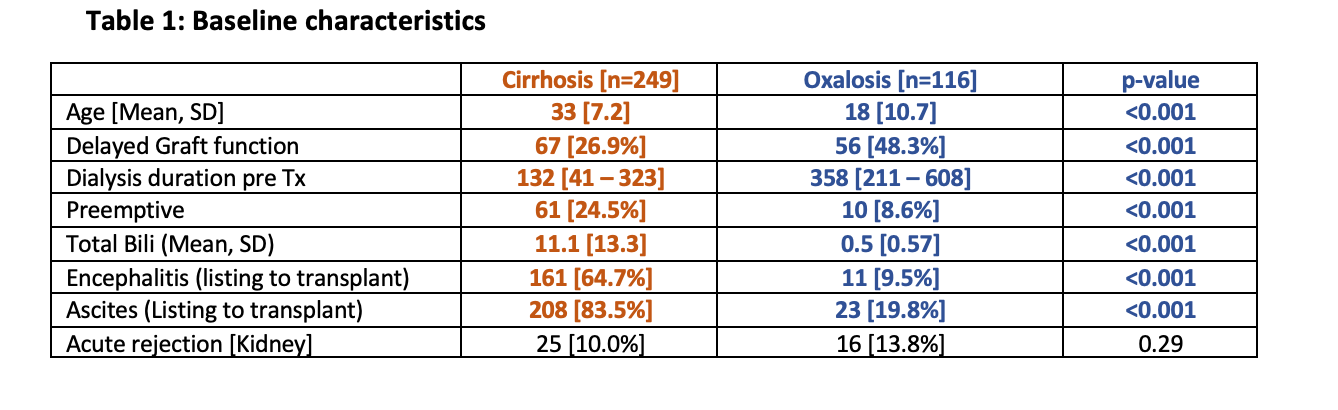
*Methods: We conducted a retrospective analysis of UNOS database (2000-2019) among SLKT recipients who had a diagnosis of Oxalosis or Cirrhosis. To prevent the selection bias, only younger patients with age<40 years were selected for the study in both groups. Graft survival time and graft failure rate were measured using Kaplan Meier analysis.
*Results: Of the total of 365 patients, 116 (31.8%) were in the Oxalosis group and the remaining 249 were in the cirrhosis group. Patients in the Oxalosis group were younger, had lower BMI, higher rate of delayed graft function (48.3% vs 26.9%, p<0.001), increased dialysis vintage time and less preemptive transplants (Table 1). There was no difference in acute rejection rates, death censored kidney graft survival at 1st, 3rd, 5th and 10th year between the groups.
*Conclusions: Among the SLKT recipients, young patients with liver cirrhosis had similar graft and patient outcomes compared to patients with metabolic liver disease, who otherwise had normal liver function pre-transplant. This could be due to shorter ESRD duration in cirrhosis patients pre-transplant. The presence of ESLD pre-transplant does not appear to affect the rate of allograft rejection in SLKT recipients.
To cite this abstract in AMA style:
Kyriazis P, Patel H, Nissaisorakarn P, Cardarelli F, Agrawal N. Comparison of Allograft Outcomes in SLK Transplant Patients with and without ESLD: A UNOS Database Analysis [abstract]. Am J Transplant. 2021; 21 (suppl 3). https://atcmeetingabstracts.com/abstract/comparison-of-allograft-outcomes-in-slk-transplant-patients-with-and-without-esld-a-unos-database-analysis/. Accessed March 2, 2026.« Back to 2021 American Transplant Congress