Identifying Health-System Level Barriers and Facilitators to Living Donor Kidney Transplantation: A Comparative Case Study
1Nephrology, McGill University Health Centre, Montreal, QC, Canada, 2Nephrology, Centre Hospitalier de l’Université de Montréal, Montreal, QC, Canada, 3Family Medicine, McGill University, Montreal, QC, Canada, 4Nephrology, University of British Columbia, Vancouver, BC, Canada
Meeting: 2021 American Transplant Congress
Abstract number: 965
Keywords: Allocation, Kidney transplantation, Living donor, Public policy
Topic: Clinical Science » Kidney » Kidney Living Donor: Other
Session Information
Session Name: Kidney Living Donor: Other
Session Type: Poster Abstract
Session Date & Time: None. Available on demand.
Location: Virtual
*Purpose: Despite the well-known advantages of living donor kidney transplantation (LDKT), rates at many centers have stagnated or declined. In Canada, there are large interprovincial variations in LDKT rates, the reasons for which are not well understood. The objective of this study is to identify health system-level barriers and facilitators to LDKT by investigating and comparing health systems.
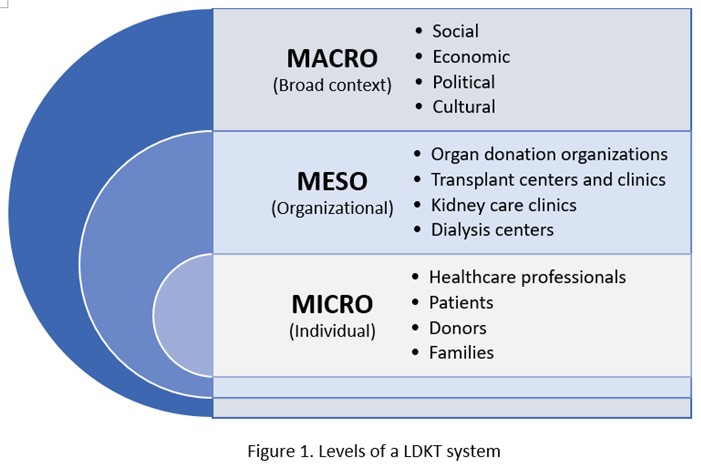
*Methods: This research takes the form of a comparative case study, which entails analyzing similarities, differences, and patterns across multiple cases. Each province presents a case. Thus, we are comparing the health systems in three provinces, where 50-60%; 30-40%; <15% of kidney transplants done annually are from living donors. Data collection involves document analysis; semi-structured interviews; participant observation. Our qualitative methodology reflects the need to understand health systems as an integrated whole - across macro, meso and micro levels - by investigating the relationships between its agents (Figure 1). Data are being analyzed using framework analysis.
*Results: We commenced research in the province with the highest rates of LDKT. Thus far we have conducted 15 interviews with personnel from various organizations involved in co-ordinating LDKT, whilst initiating document analysis of organizational guidelines, policies and resources. Preliminary themes from this province reveal: 1) Efforts to increase LDKT are not only focused on micro levels; 2) Strong links exist between multiple levels of practice – macro, meso and micro – that are involved in facilitating LDKT; 3) Professional networks and working groups span the core to periphery of renal practices in the province; 4) These groups have developed educational initiatives and standardized resources related to LDKT; 5) These efforts facilitate buy-in to LDKT as a treatment option across the province.
*Conclusions: Preliminary results suggest that in order to increase rates of LDKT in lower-performing provinces, interventions must target the dynamic relationships between different elements of a system. This contradicts current efforts that primarily target barriers on the micro-level (i.e. the patient). Thus, efforts to increase LDKT, must target multiple levels of practice in order improve access and capacity for LDKT.
To cite this abstract in AMA style:
Horton A, Fortin M, Nugus P, Landsberg D, Paquet M, Cantarovich M, Sandal S. Identifying Health-System Level Barriers and Facilitators to Living Donor Kidney Transplantation: A Comparative Case Study [abstract]. Am J Transplant. 2021; 21 (suppl 3). https://atcmeetingabstracts.com/abstract/identifying-health-system-level-barriers-and-facilitators-to-living-donor-kidney-transplantation-a-comparative-case-study/. Accessed March 1, 2026.« Back to 2021 American Transplant Congress