Survival After Heart Transplant vs. Simultaneous Heart Kidney Transplant by Degrees of Renal Dysfunction at Engraftment in the United States: A Multivariable Analysis
1Medicine, University of Minnesota, Eden Prairie, MN, 2Complex Care Analytics, Fairview Health Services, Minneapolis, MN, 3Transplant, Mayo Clinic, Jacksonville, FL, 4Surgery, University of Minnesota, Minneapolis, MN
Meeting: 2021 American Transplant Congress
Abstract number: LB 18
Keywords: Allocation, Multivisceral transplantation, Survival
Topic: Clinical Science » Heart » Heart and VADs: All Topics
Session Information
Session Name: Late Breaking: All Organs
Session Type: Rapid Fire Oral Abstract
Date: Tuesday, June 8, 2021
Session Time: 6:00pm-7:00pm
 Presentation Time: 6:05pm-6:10pm
Presentation Time: 6:05pm-6:10pm
Location: Virtual
*Purpose: There has been a rising trend for utilizing kidneys in heart transplant candidates with different renal dysfunction degrees without established criteria to address this utility.
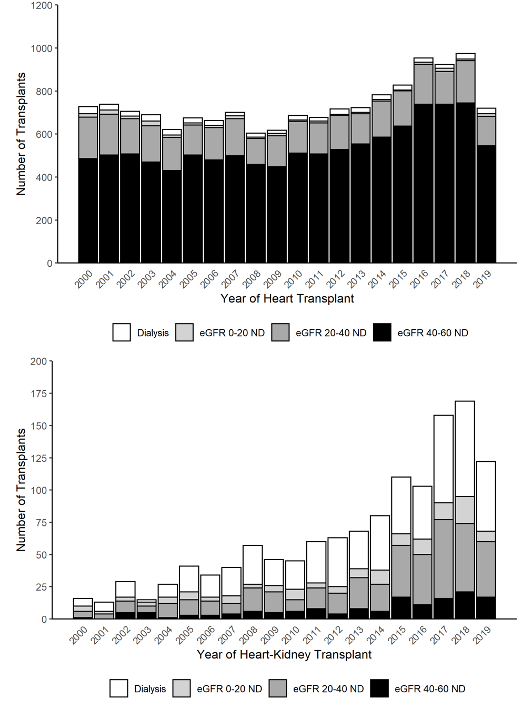
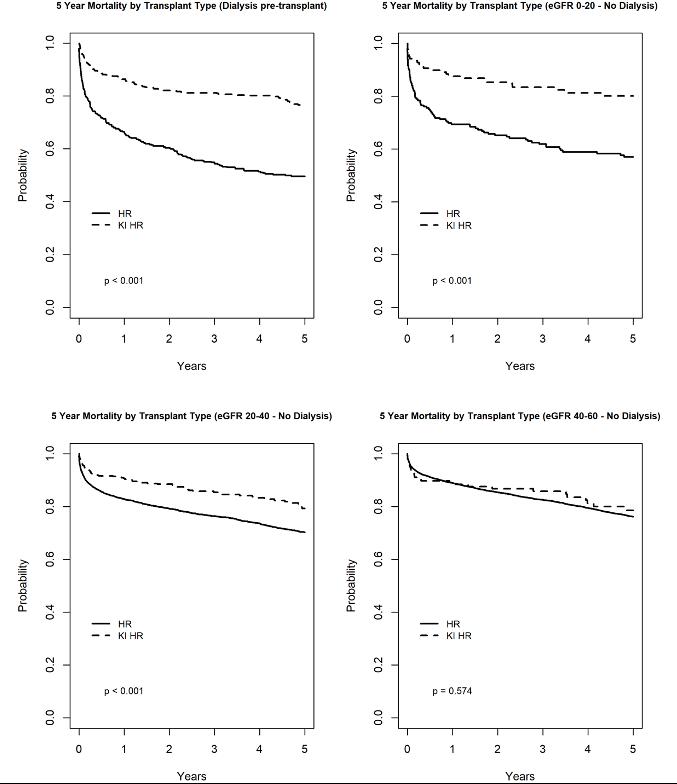
*Methods: We analyzed the SRTR between 1/1/2000 and 9/31/2019. We identified all primary adult heart transplant recipients (HAT) and simultaneous heart kidney transplants (SHK). We sorted the recipients into four groups based on the degree of renal dysfunction at the time of transplantation: dialysis group, eGFR <20, eGFR 20-40 and eGFR>40-60 mL/min. Kaplan-Meier curves were generated to compare mortality by transplant type among the four groups. We analyzed predictors of mortality in each of the four groups separately. We used Cox proportional hazard models adjusted for recipient age, gender, race, diabetes status, heart transplant indication, ICU status, waiting time in weeks, transplant year, donor age, local vs. import organs, heart ischemia time and payor type. Follow-up was censored at five years post-transplant.
*Results: Of the recipients with eGFR60 mL/min 14,728 received (HAT) and 1296 received (SHK). The proportion of SHK increased from 3% to 15% of all heart recipients over the study period. The proportion of SHK recipients with reasonably good renal function (>40-60 mL/min) before transplantation was 11.3%. In the multivariable Cox regression model for recipients in the eGFR >40-60 mL/min group, there was no survival benefit to SHK as compared to HAT (LLCI, aHR, ULCI) (0.61, 0.92,1.39).In the lower the GFR groups, compared to HAT, SHK was associated with 35% better survival in the eGFR 20-40 mL/min group (0.49, 0.65, 0.85), 68% improved survival (0.18, 0.32,0.57) in the eGFR<20 mL/min group and 55% improved survival (0.34, 0.45, 0.58) in the dialysis group.
*Conclusions: Utilizing kidneys in heart transplant recipients with eGFR > 40 mL/min at the time of transplantation is an unwarranted use of a scarce resource.
To cite this abstract in AMA style:
Riad SM, Aljuhani M, Jackson S, Alexy T, Wadie H, Martin C, Kandaswamy R. Survival After Heart Transplant vs. Simultaneous Heart Kidney Transplant by Degrees of Renal Dysfunction at Engraftment in the United States: A Multivariable Analysis [abstract]. Am J Transplant. 2021; 21 (suppl 3). https://atcmeetingabstracts.com/abstract/survival-after-heart-transplant-vs-simultaneous-heart-kidney-transplant-by-degrees-of-renal-dysfunction-at-engraftment-in-the-united-states-a-multivariable-analysis/. Accessed February 17, 2026.« Back to 2021 American Transplant Congress