Characteristics of Incisional Hernia Development after Live Donor Nephrectomy: Impact of Surgical Technique
1Surgery, Vanderbilt University Medical Center, Nashville, TN, 2Vanderbilt University School of Medicine, Nashville, TN
Meeting: 2020 American Transplant Congress
Abstract number: D-045
Keywords: Post-operative complications
Session Information
Session Name: Poster Session D: Kidney Living Donor: Long Term Outcomes
Session Type: Poster Session
Date: Saturday, May 30, 2020
Session Time: 3:15pm-4:00pm
 Presentation Time: 3:30pm-4:00pm
Presentation Time: 3:30pm-4:00pm
Location: Virtual
*Purpose: The characteristics of incisional hernia (IH) formation following live donor nephrectomy (LDN) are not well defined. The goal of the present study was to define the incidence of IH following LDN and identify potential risk factors contributing to their formation.
*Methods: We performed a single center, retrospective review of all LDN between February 2013 to October 2018. Patients with and without IH development were compared based on donor and operative variables. A univariate analysis was completed to identify potential risk factors for hernia formation. A p value of < 0.05 was considered significant.
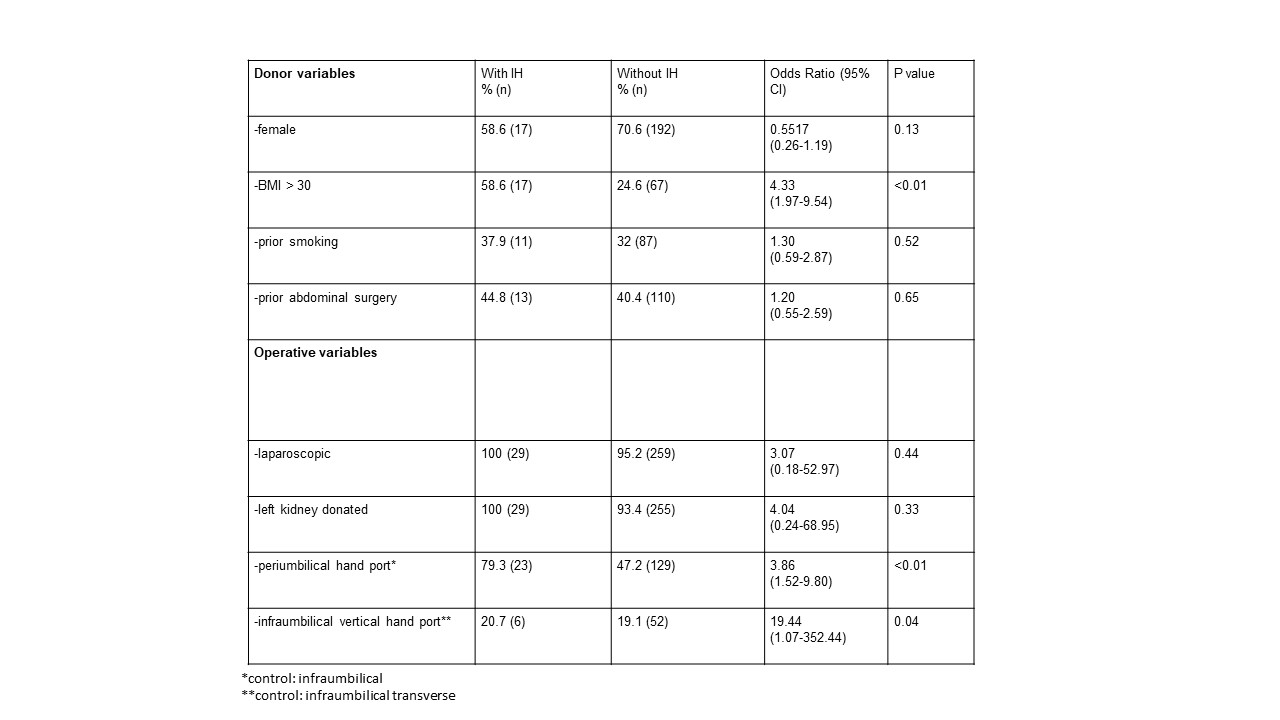
*Results: 301 individuals underwent live donor nephrectomy during the study period. 288 were performed laparoscopically with a hand-assist technique. 152 cases utilized a periumbilical handport, whereas 136 were performed through an infraumbilical handport. Infraumbilical handports were placed through either a vertical (58) or transverse (78) fascial incision. 29 patients (9.6%) developed an incisional hernia with median time to development of 8 months (range: 2-51 months). 2 cases (6.9%) required emergent repair. BMI > 30 was associated with an increased risk of hernia formation (odds ratio [OR] 4.33, 95% confidence interval [CI]: 1.97-9.54, p <0.01). The periumbilical handport (OR 3.86, 95% CI: 1.52-9.8, p <0.01) and infraumbilical vertical fascial handport (OR 19.44, 95% CI: 1.07-352.44, p=0.04) were associated with hernia formation.
*Conclusions: The incidence of IH following LDN is significant and impacted by surgical technique. Placing the handport infraumbilical with a transverse fascial incision may reduce the risk of hernia formation following LDN.
To cite this abstract in AMA style:
DuBray BJ, Thompson JJ, Forbes RC. Characteristics of Incisional Hernia Development after Live Donor Nephrectomy: Impact of Surgical Technique [abstract]. Am J Transplant. 2020; 20 (suppl 3). https://atcmeetingabstracts.com/abstract/characteristics-of-incisional-hernia-development-after-live-donor-nephrectomy-impact-of-surgical-technique/. Accessed February 27, 2026.« Back to 2020 American Transplant Congress