Access to and Survival Benefit of Kidney Transplantation in Patients with Sickle Cell Disease-Associated End-Stage Renal Disease in the United States
Johns Hopkins School of Medicine, Baltimore, MD
Meeting: 2020 American Transplant Congress
Abstract number: C-237
Keywords: Survival
Session Information
Session Name: Poster Session C: Non-Organ Specific: Disparities to Outcome and Access to Healthcare
Session Type: Poster Session
Date: Saturday, May 30, 2020
Session Time: 3:15pm-4:00pm
 Presentation Time: 3:30pm-4:00pm
Presentation Time: 3:30pm-4:00pm
Location: Virtual
*Purpose: Patients with end-stage renal disease due to sickle cell disease (SCD-ESRD) have high mortality, which might be reduced by kidney transplantation (KT). However, whether KT is desirable in SCD-ESRD patients is controversial, potentially limiting their access to KT, because SCD-ESRD KT recipients may experience higher mortality than other KT recipients. Survival benefit, or reduction in mortality associated with KT, is unknown in SCD-ESRD patients. We aimed to quantify survival benefit of KT and to compare the access to KT in SCD-ESRD versus non-SCD-ESRD patients.
*Methods: Using USRDS and SRTR data, we studied adult SCD-ESRD and non-SCD-ESRD patients who began routine dialysis or were added to the national KT waitlist in 1998-2017. To quantify survival benefit, we created SCD and non-SCD matched pairs (SCD KT recipient and SCD waitlisted candidate; and non-SCD KT recipient and non-SCD waitlisted candidate) using sequential stratification. Survival benefit of KT was defined as reduction in mortality associated with receiving KT versus remaining on dialysis awaiting KT, measured in both absolute risk difference and hazard ratio (HR) for mortality. To compare the access to KT, we estimated HRs for receiving KT in SCD-ESRD versus non-SCD-ESRD patients, treating death as a competing risk.
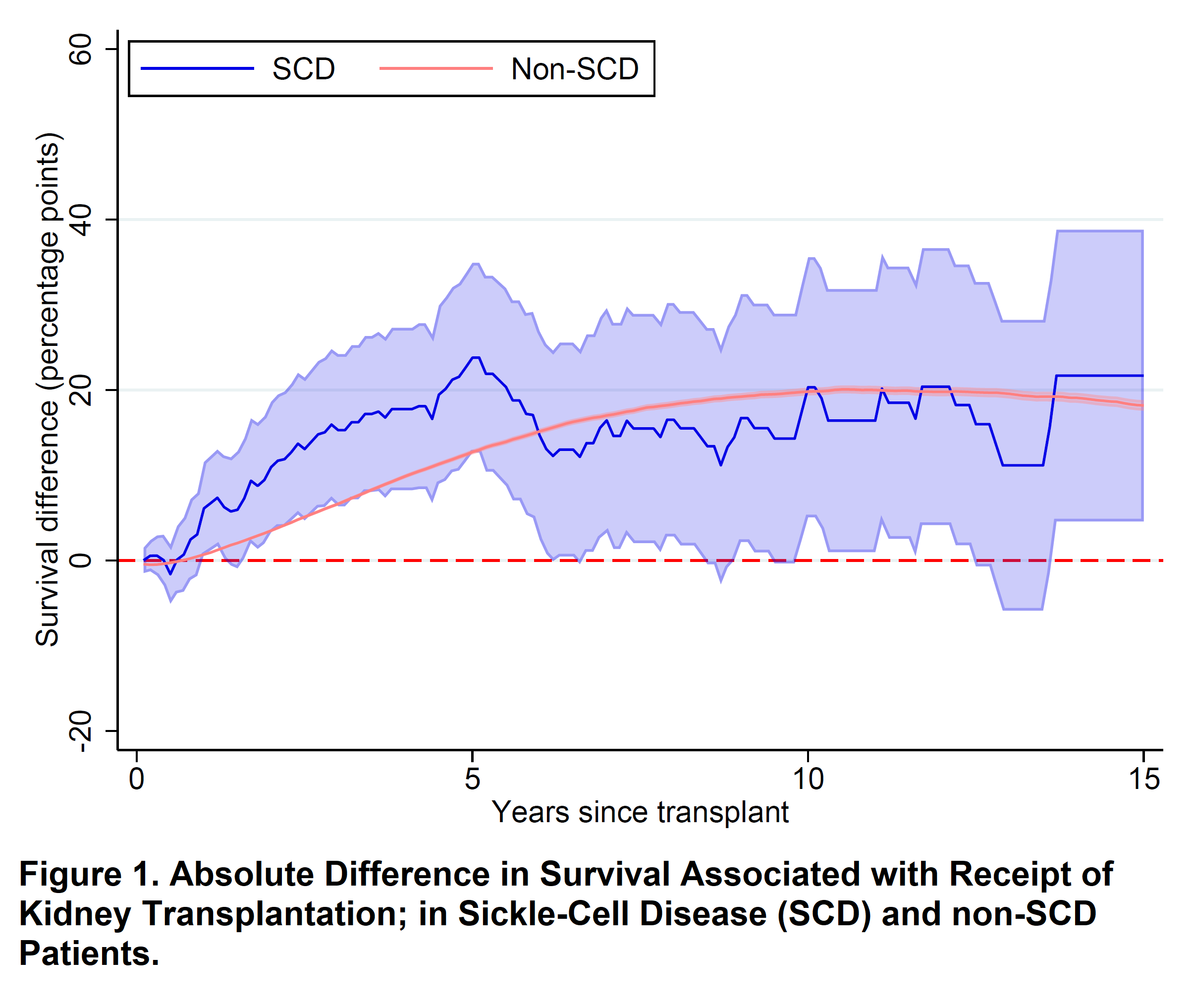
*Results: Among 189 SCD and 220,251 non-SCD KT recipients matched to waitlisted candidates, KT was associated with decreased mortality. Absolute risk difference was 0.920.339.8 percentage-points (PP) in SCD and 19.219.820.4 PP in non-SCD patients at 10-year post-KT. HR was 0.360.570.91 in SCD and 0.530.540.55 in non-SCD patients; these HRs did not differ between SCD and non-SCD patients (interaction p=0.8). Nonetheless, SCD-ESRD patients were less likely to receive KT than non-SCD-ESRD patients (subdistribution HR=0.610.730.87). Similar disparities were found among waitlisted candidates (subdistribution HR=0.530.620.72), even after accounting for differences in mortality and factors constituting the kidney allocation criteria (cause-specific HR=0.710.820.94).
*Conclusions: SCD-ESRD and non-ESRD populations received similar survival benefit from KT. Nonetheless, SCD-ESRD patients were less likely to receive KT, even after waitlist registration. Our findings suggest that access to KT should be improved for SCD-ESRD patients.
To cite this abstract in AMA style:
Bae S, Johnson M, Massie A, Luo X, Jr CHaywood, Lanzkron S, Grams M, Segev D, Purnell T. Access to and Survival Benefit of Kidney Transplantation in Patients with Sickle Cell Disease-Associated End-Stage Renal Disease in the United States [abstract]. Am J Transplant. 2020; 20 (suppl 3). https://atcmeetingabstracts.com/abstract/access-to-and-survival-benefit-of-kidney-transplantation-in-patients-with-sickle-cell-disease-associated-end-stage-renal-disease-in-the-united-states/. Accessed February 27, 2026.« Back to 2020 American Transplant Congress