Individualized Impact of Donation after Cardiac Death on Kidney Transplant Outcomes
Johns Hopkins School of Medicine, Baltimore, MD
Meeting: 2020 American Transplant Congress
Abstract number: C-025
Keywords: Donors, non-heart-beating
Session Information
Session Name: Poster Session C: Kidney Deceased Donor Selection
Session Type: Poster Session
Date: Saturday, May 30, 2020
Session Time: 3:15pm-4:00pm
 Presentation Time: 3:30pm-4:00pm
Presentation Time: 3:30pm-4:00pm
Location: Virtual
*Purpose: Increasing the use of kidneys from donation after cardiac death (DCD) donors is a potential solution to mitigate the current organ shortage. However, DCD kidneys may lead to worse outcomes compared to kidneys donated after brain death (DBD), especially when the donor or the recipient has higher risk. It is crucial to understand in what clinical circumstances DCD kidneys can be safely transplanted with minimal harms. Thus, we aimed to model the impact of DCD as a function of clinical variables, and to provide candidate-specific prediction of the risk associated with DCD transplantation.
*Methods: Using SRTR data, we studied adult deceased-donor kidney transplant (KT) recipients in 2007-2018. We measured the association of DCD (vs. DBD) with death-censored graft failure and patient death using stratified Cox models. We included interaction terms of DCD and clinical factors to model the association of DCD as a function of the clinical factors. Clinical factors were selected using the LASSO regularization.
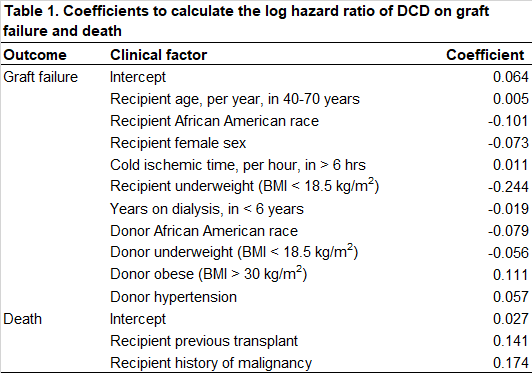
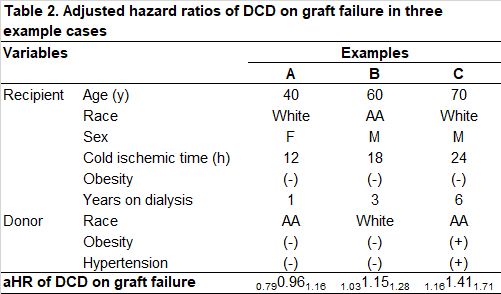
*Results: Of the 125,510 recipients included in our study, 22,251 (17.7%) received kidneys from DCD donors. Overall, DCD was associated with increased hazard of graft failure (aHR=1.151.211.28) and death (aHR=1.021.061.11). This association of DCD with increased graft failure was stronger among recipients with older age and longer cold ischemic time, and among donors with obesity and hypertension. Conversely, this association was weaker among recipients with African American race, female sex, underweightness, and longer time on dialysis (up to 6 years), and donors with African American race and underweightness (Table 1). Combined together, our model predicted that DCD would have no impact on graft failure in some cases (Table 2; Example A), but could significantly increase graft failure in others (Table 2; Examples B and C). The association of DCD with death had smaller variation; it was stronger among recipients with previous transplants and history of malignancy (Table 1). We also created an online calculator based on our models (http://www.transplantmodels.com/dcd_impact).
*Conclusions: The negative impact of DCD on KT outcomes differs between patients. Our model can identify KT candidates who may safely receive DCD kidneys with minimal risk.
To cite this abstract in AMA style:
Bae S, Massie A, Wang JGaronzik, Segev D. Individualized Impact of Donation after Cardiac Death on Kidney Transplant Outcomes [abstract]. Am J Transplant. 2020; 20 (suppl 3). https://atcmeetingabstracts.com/abstract/individualized-impact-of-donation-after-cardiac-death-on-kidney-transplant-outcomes/. Accessed February 5, 2026.« Back to 2020 American Transplant Congress