Medication Knowledge Retention and Adherence Following Transplant: Is There Room for Improvement?
M. H. Cooper1, A. W. Rogers1, T. L. Menser2, J. C. Krisl1
1Department of Pharmacy, Houston Methodist Hospital, Houston, TX, 2Houston Methodist Research Institute, Houston Methodist Hospital, Houston, TX
Meeting: 2020 American Transplant Congress
Abstract number: B-237
Keywords: Immunosuppression, Outpatients, Patient education
Session Information
Session Name: Poster Session B: Psychosocial and Treatment Adherence
Session Type: Poster Session
Date: Saturday, May 30, 2020
Session Time: 3:15pm-4:00pm
 Presentation Time: 3:30pm-4:00pm
Presentation Time: 3:30pm-4:00pm
Location: Virtual
*Purpose: Transplant recipients’ complex medication regimens following transplant can lead to non-adherence, which has been linked to increased rates of acute rejection and graft loss. In this study, we assessed medication knowledge retention and its impact on adherence in transplant patients following index discharge.
*Methods: We performed a single-center, retrospective chart review of all English literate adults transplanted from April 1 to October 30, 2019 seen for initial clinic visits. The primary endpoint was medication knowledge retention and adherence following discharge, assessed through an original medication knowledge questionnaire and the immunosuppressant therapy adherence scale, respectively. The measurement of outcomes included: medication comfortability (1 to 5), knowledge (0 to 1), and adherence (0 to 12). Baseline measures were obtained by the second clinic visit and follow-up measurement was within 3 months post-transplant.
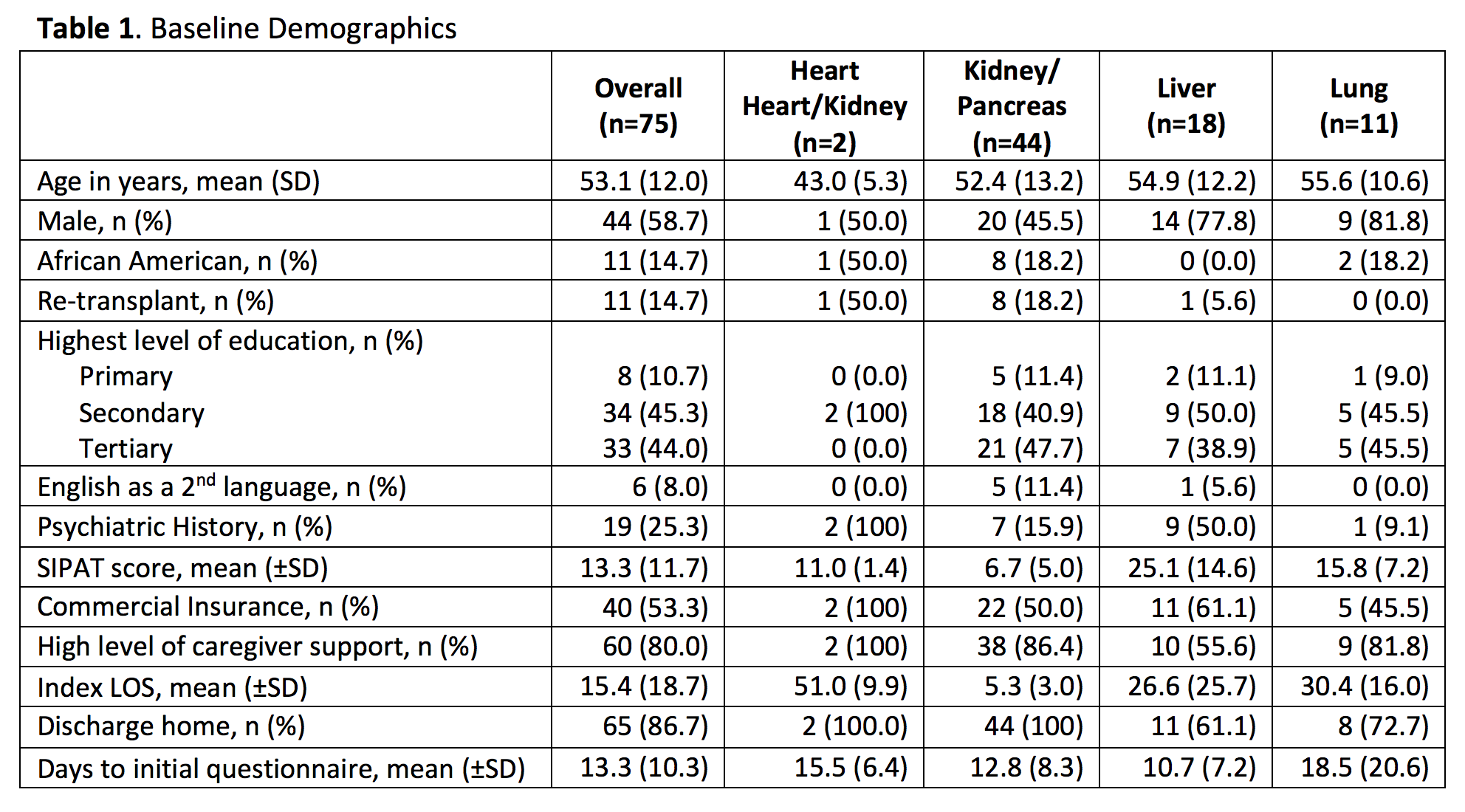
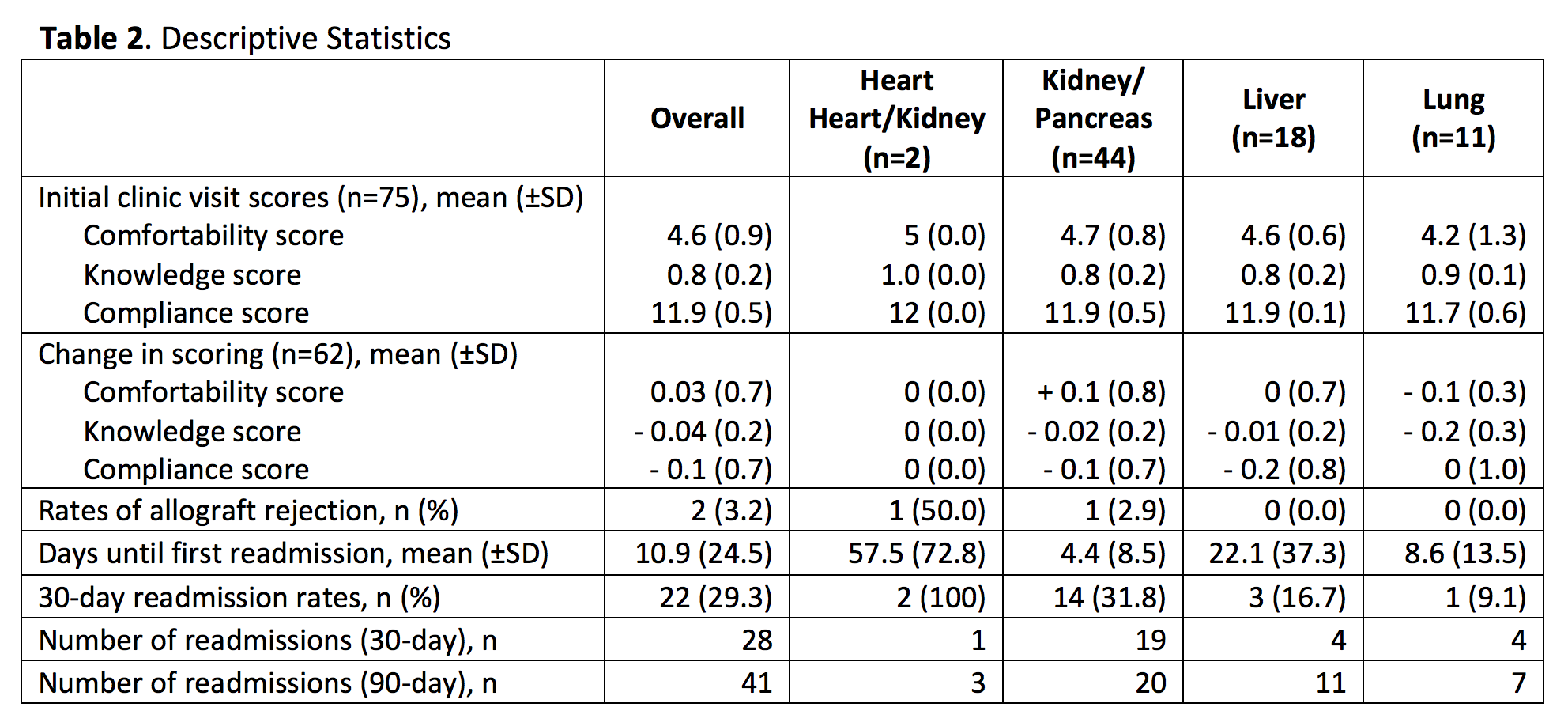
*Results: A total of 112 transplant recipients were identified, of which 37 and 50 were excluded (n=75 and n=62). Baseline demographics are reported in Table 1. Baseline comfortability, knowledge, and adherence scores were 4.6/5 (92.0%), 0.8/1 (80.0%), and 11.9/12 (99.2%), respectively; the change in each respective score was +0.03, -0.04, and -0.1. The largest negative change was observed in the liver and lung recipients, which was driven by the reduced adherence scores amongst the liver recipients, while a decrease in medication knowledge was the primary cause of decline for the lung recipients. Our data suggests that medication knowledge and adherence are initially high, but both decline with time following transplant. Additional outcomes are reported in Table 2.
*Conclusions: Our findings suggest that medication education should extend past the time of initial discharge, thus warranting the expansion of pharmacy services for ongoing patient education in the outpatient setting. Reinforcement of inpatient education practices are likely particularly important for those identified with low level of caregiver support and lower health literacy.
To cite this abstract in AMA style:
Cooper MH, Rogers AW, Menser TL, Krisl JC. Medication Knowledge Retention and Adherence Following Transplant: Is There Room for Improvement? [abstract]. Am J Transplant. 2020; 20 (suppl 3). https://atcmeetingabstracts.com/abstract/medication-knowledge-retention-and-adherence-following-transplant-is-there-room-for-improvement/. Accessed February 22, 2026.« Back to 2020 American Transplant Congress