Living Donor versus Deceased Donor Liver Transplantation in USA: Where Do We Stand, Where to Go
1Henry Ford Hospital, Detroit, MI, 2University of Chicago Medical Center, Chicago, IL
Meeting: 2020 American Transplant Congress
Abstract number: B-165
Keywords: Living donor, Survival, Waiting lists
Session Information
Session Name: Poster Session B: Liver: Living Donors and Partial Grafts
Session Type: Poster Session
Date: Saturday, May 30, 2020
Session Time: 3:15pm-4:00pm
 Presentation Time: 3:30pm-4:00pm
Presentation Time: 3:30pm-4:00pm
Location: Virtual
*Purpose: LDLT represents a very small percentage of all liver transplants done in the United States, despite the shortage of deceased donor organs. The aim of this study was to compare outcomes between living donor liver transplant (LDLT) and deceased donor liver transplant (DDLT) over a large patient population using the UNOS database. In addition, we studied possible challenges.
*Methods: This was a retrospective analysis comparing LDLT versus DDLT in the period between January 2008 and December 2017 using the UNOS database.
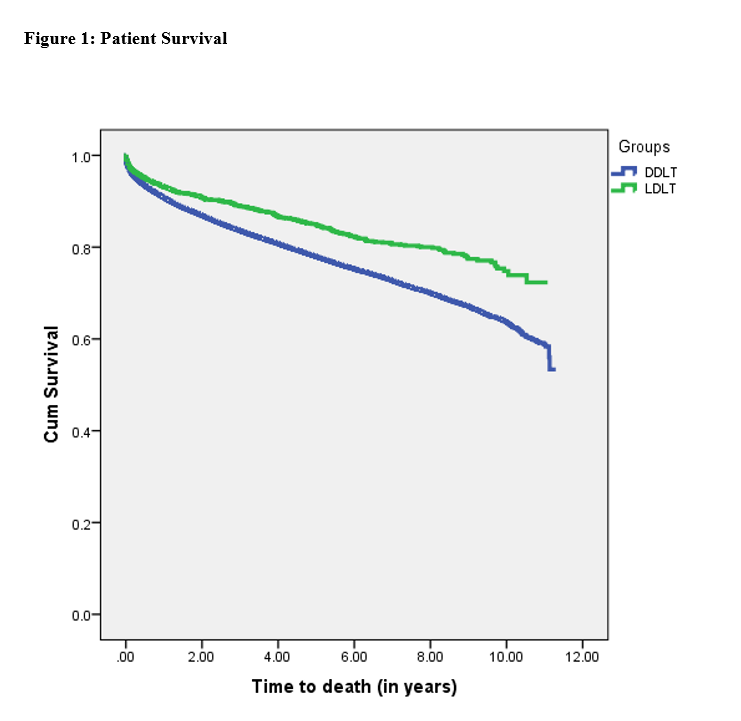
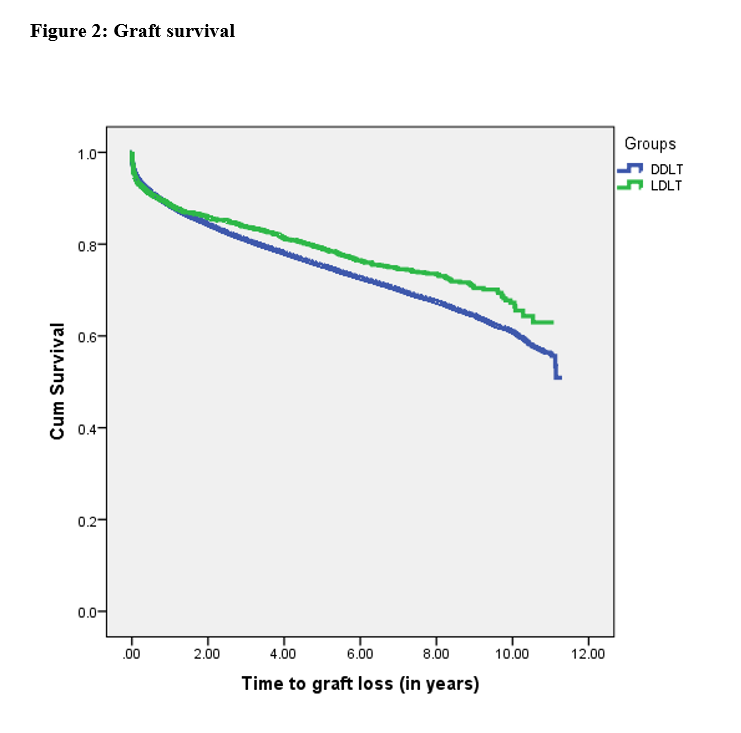
*Results: 61924 cases were studied, LDLT group included 2846 and DDLT group included 59078 cases. Median age for LDLT group was 52 versus 56 year for DDLT group (P=0.0001). Median waiting time for LDLT was 0.36 versus 1.78 year in DDLT (P=0.0001). Median MELD score for LDLT group was 15 versus 20 for DDLT group (P=0.0001). HLA data were found in 23143 cases. Median HLA mismatch level was 3 in LDLT group versus 5 in DDLT group (P=0.0001). Data about recipient education level were found in 53911 cases. 36.7% were highly educated in LDLT group versus 24.5% in DDLT group (P=0.0001). Regions with higher percentage of LDLT were not matching regions with longer waiting time. The 3-, 5-, and 10-year patient survival for LDLT group was 87%, 82%, and 72% versus 81%, 75%, and 58% for DDLT group (P = 0.0001). The 3-, 5-, and 10-year graft survival for LDLT group was 81%, 76%, and 63% versus 78%, 72%, and 56% for DDLT group (P = 0.0001). Live liver donation stayed independent predictor of graft survival after modifying risk for adult vs pediatric, gender, race using cox regression (P= 0.040). There was no significant difference in median hospital stay (11 days in LDLT group vs 10 days in DDLT group, P=0.071).
*Conclusions: LDLT offers advantages over DDLT including better graft and patient survival, less resource utilization by decrease waiting time. The time has come to change the justification of the importance of LDLT development in this country. LDLT was used more in well-educated recipients implicating the importance of awareness spread about live liver donation. Long waiting time in some regions did not necessitate increase numbers of LDLT. The main challenge for LDLT expansion is population and medical teams’ education.
To cite this abstract in AMA style:
Elsabbagh AM, Yoshida A, Fung J, Abouljoud M. Living Donor versus Deceased Donor Liver Transplantation in USA: Where Do We Stand, Where to Go [abstract]. Am J Transplant. 2020; 20 (suppl 3). https://atcmeetingabstracts.com/abstract/living-donor-versus-deceased-donor-liver-transplantation-in-usa-where-do-we-stand-where-to-go/. Accessed February 19, 2026.« Back to 2020 American Transplant Congress