Post-Transplant Collagen I and Collagen III Antibodies and Antibody-Mediated Rejection in Kidney Transplantation Recipients
1Armed Forces Capital Hospital, Gyeonggi-do, Korea, Republic of, 2Seoul National University Hospital, Seoul, Korea, Republic of
Meeting: 2020 American Transplant Congress
Abstract number: B-072
Keywords: Antibodies, Kidney transplantation, Rejection
Session Information
Session Name: Poster Session B: Kidney Chronic Antibody Mediated Rejection
Session Type: Poster Session
Date: Saturday, May 30, 2020
Session Time: 3:15pm-4:00pm
 Presentation Time: 3:30pm-4:00pm
Presentation Time: 3:30pm-4:00pm
Location: Virtual
*Purpose: An emerging role of non-human leukocyte antigen (HLA) antibodies on the risk of antibody-mediated rejection (AMR) has been suggested, although most of their non-HLA antigens remain poorly defined. We explored the association of HLA and non-HLA antibodies and AMR in kidney transplantation recipients.
*Methods: The study included transplant recipients in one of the tertiary hospitals in Korea. We collected post-transplant sera from 51 kidney transplant recipients when biopsies revealing AMR were performed. As a control group without rejection, 49 post-transplant sera from transplant recipients without rejection and as a T-cell mediated rejection control group, 45 sera from patients with T-cell mediated rejection but without AMR were included. The titers of non-HLA antibodies were measured by the Luminex, LABScreen Autoantibody (One Lambda) and reported as mean fluorescence intensity values. We measured the titers of 41 non-HLA antibodies that are potentially associated with AMR, and several known antibodies, including angiotensin receptor type 1 (AT1R) antibody and MHC class I polypeptide-related sequence A (MICA) antibody.
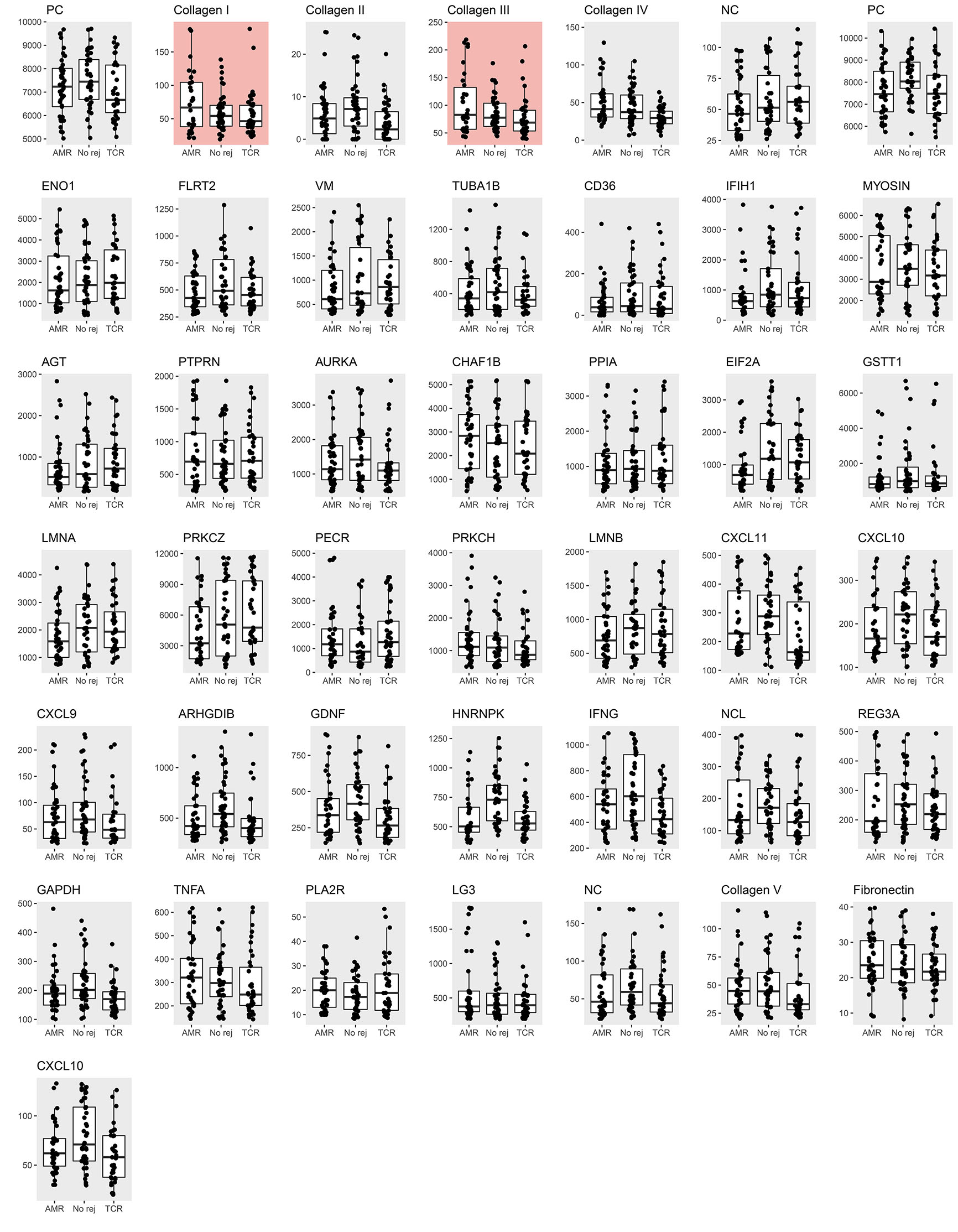
*Results: The baseline characteristics of the AMR group and the control groups were relatively similar, except for that the AMR cases were diagnosed in the later periods from transplantation and had a higher proportion of HLA mismatched cases and cases with positive donor-specific antibody. The titers of collagen I and collagen III antibodies were significantly higher in the AMR cases, both when compared to the no rejection group and the T-cell mediated rejection only group. The titers of collagen I and collagen III antibodies did not differ according to the presence of DSA or other diagnosis within the AMR group. Among the AMR cases, those with higher titers of collagen I or collagen III antibody had more severe degrees of peritubular capillaritis. When we performed a multivariable analysis, even after adjusting the presence of donor-specific antibody, AT1R, and MICA sensitized state, which were significantly associated with the odds for AMR, the presence of high (> 75 percentile) collagen I antibody titer [adjusted odds ratio 8.29 (2.92-25.66)] and collagen III antibody titer [adjusted odds ratio 11.74 (3.86-40.28)] were also significantly associated with the odds for AMR.
*Conclusions: Post-transplant collagen I and collagen III antibodies may be novel non-HLA antibodies that are related to AMR of kidney allograft.
To cite this abstract in AMA style:
Park S, Yang S, Kim J, Kim Y, Kim Y, Ha J, Moon K, Song E, Lee H. Post-Transplant Collagen I and Collagen III Antibodies and Antibody-Mediated Rejection in Kidney Transplantation Recipients [abstract]. Am J Transplant. 2020; 20 (suppl 3). https://atcmeetingabstracts.com/abstract/post-transplant-collagen-i-and-collagen-iii-antibodies-and-antibody-mediated-rejection-in-kidney-transplantation-recipients/. Accessed February 18, 2026.« Back to 2020 American Transplant Congress