Liver Retransplantation (reLT) in the Modern Post-MELD, Post-DAA Era
School of Medicine, UCSF, San Francisco, CA
Meeting: 2020 American Transplant Congress
Abstract number: 374
Keywords: Retransplantation
Session Information
Session Name: Liver Retransplantation and Other Complications
Session Type: Oral Abstract Session
Date: Saturday, May 30, 2020
Session Time: 3:15pm-4:45pm
 Presentation Time: 4:15pm-4:27pm
Presentation Time: 4:15pm-4:27pm
Location: Virtual
*Purpose: Liver retransplantation (reLT) is responsible for a small proportion of all liver transplants (LT), but outcomes are much worse than primary LT. Hepatitis C recurrence as the indication for reLT has decreased with the advent of direct acting antivirals (DAA). The purpose of this study is to characterize reLT in the modern era, and identify differences in outcomes after reLT over time, across different eras.
*Methods: We retrospectively analyzed data from UNOS for adults undergoing first reLT from 2/27/02-12/31/17. Patients were compared across three eras: 1 (2002-6), 2 (2007-11), and 3 (2012-17) and according to HCV status. Primary outcome is patient survival.
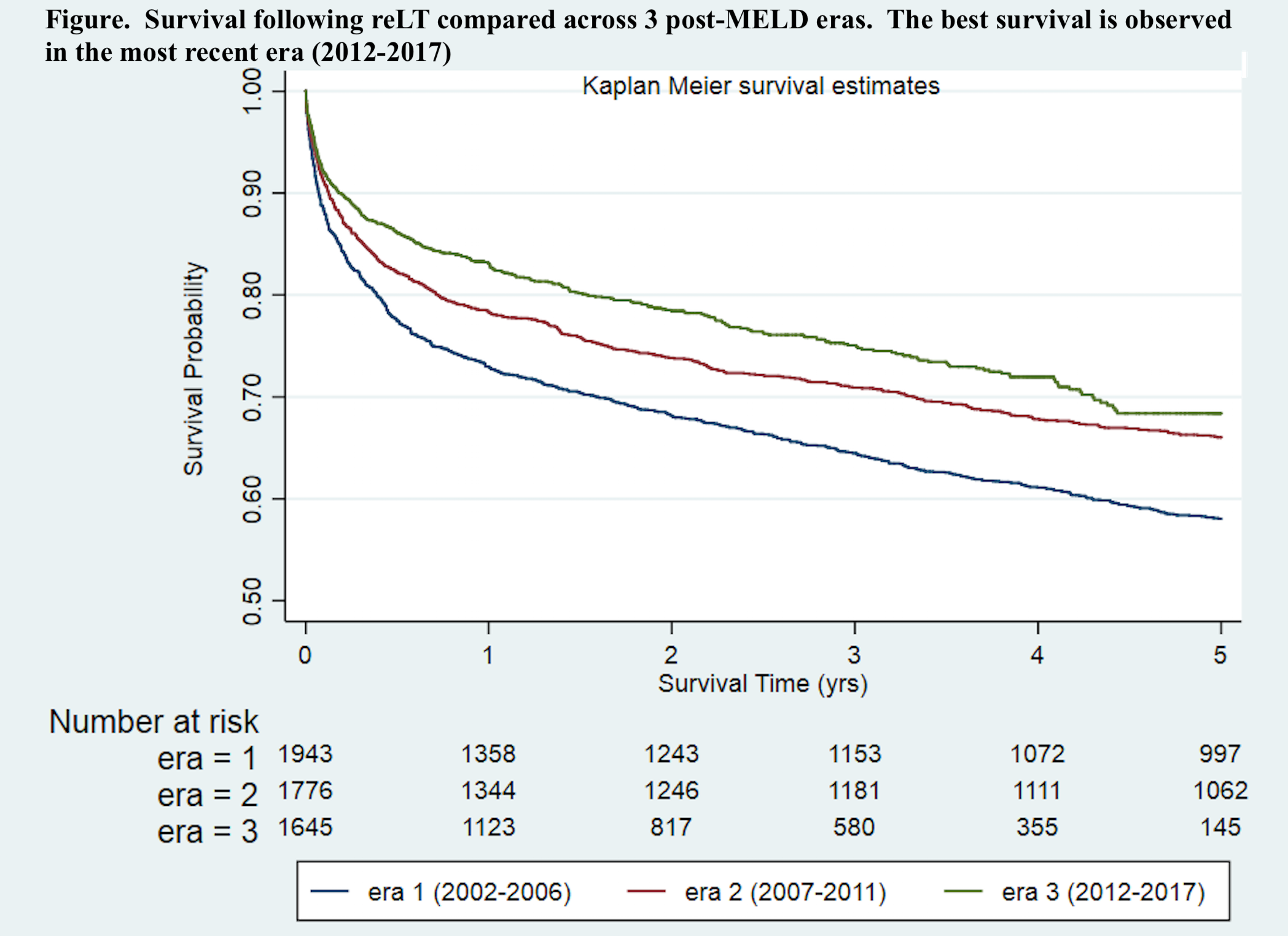
*Results: Of 5483 reLT identified, 1991 occurred in era 1, 1819 in era 2 and 1680 in era 3. Median age was 52, 34% were women, and 34% had HCV as indication for primary LT. Median time from 1st LT to reLT was 355 days. Differences between the three eras included older patients at reLT (era 3 median age=53) and increased median time to reLT (era 3 median=594 days). ReLT indications were most commonly vascular complications and HCV. Third most common reLT indication was rejection in eras 1 and 2, and non-hepatitis recurrent disease in era 3. Recurrent HCV in original graft also decreased from 19% in era 1 and 20% in era 2 to 14% in era 3 (p<0.01). MELD exception status became more common from era 1 to 3 (12 vs 17 vs 28%; p<0.01) and calculated MELD-Na at reLT was higher (27 vs 28 vs 30; p<0.01). Donor quality was better in more recent eras (donor risk index (DRI) 1.4 vs 1.3 vs 1.3; p=0.03). Post reLT survival improved across eras at 1, 3, and 5-years: 73, 64, and 58% in era 1; 78, 71, and 66% in era 2; and 83, 75, and 68% for era 3 (logrank, p<0.01). Patients with recurrent HCV at reLT had worse survival at 1, 3, and 5 years (74, 65, 58%) compared to those who did not (78, 71, 65%) (logrank, p<0.01). In multivariate cox regression, age, recurrent HCV, MELD-Na at reLT, illness severity (i.e. on mechanical ventilation, in the ICU), diabetes mellitus (DM), and DRI were associated with worse post reLT mortality, and era remained a predictor of improved mortality. ICU status and DRI remained significant predictors of mortality, regardless of era or HCV status. MELD exception status was associated with improved post reLT mortality only in era 3.
*Conclusions: Need for reLT has decreased over time, particularly with regard to recurrent HCV, with improved post reLT survival. Factors have been identified (recipient DM and DRI) which could be important in determining optimal candidates for reLT, in light of the growing population with DM and NAFLD.
To cite this abstract in AMA style:
Shi B, Freise C, Brandman D. Liver Retransplantation (reLT) in the Modern Post-MELD, Post-DAA Era [abstract]. Am J Transplant. 2020; 20 (suppl 3). https://atcmeetingabstracts.com/abstract/liver-retransplantation-relt-in-the-modern-post-meld-post-daa-era/. Accessed February 16, 2026.« Back to 2020 American Transplant Congress