The Impact of Non-Directed Anonymous Live Liver Donors on the Number of Children on the Waitlist at a Single Pediatric Liver Transplant Center
1Transplant Surgery, University of Colorado, Aurora, CO, 2Pediatric Hepatology, University of Colorado, Aurora, CO, 3Transplant Hepatology, University of Colorado, Aurora, CO
Meeting: 2020 American Transplant Congress
Abstract number: 366
Keywords: Liver grafts, Living donor, Outcome, Pediatric
Session Information
Session Name: Liver: Living Donors and Partial Grafts I
Session Type: Oral Abstract Session
Date: Saturday, May 30, 2020
Session Time: 3:15pm-4:45pm
 Presentation Time: 4:03pm-4:15pm
Presentation Time: 4:03pm-4:15pm
Location: Virtual
*Purpose: Since the initiation of our living donor (LD) pediatric liver transplant program in November 2016, 10 non-directed anonymous donors have been approved and completed live liver donation to pediatric recipients. The aim of this study was to evaluate the impact of these donors on the pediatric waitlist.
*Methods: We retrospectively reviewed all first time pediatric liver transplant candidates listed between 2012 and 2019. Continuous variables are reported as median (range).
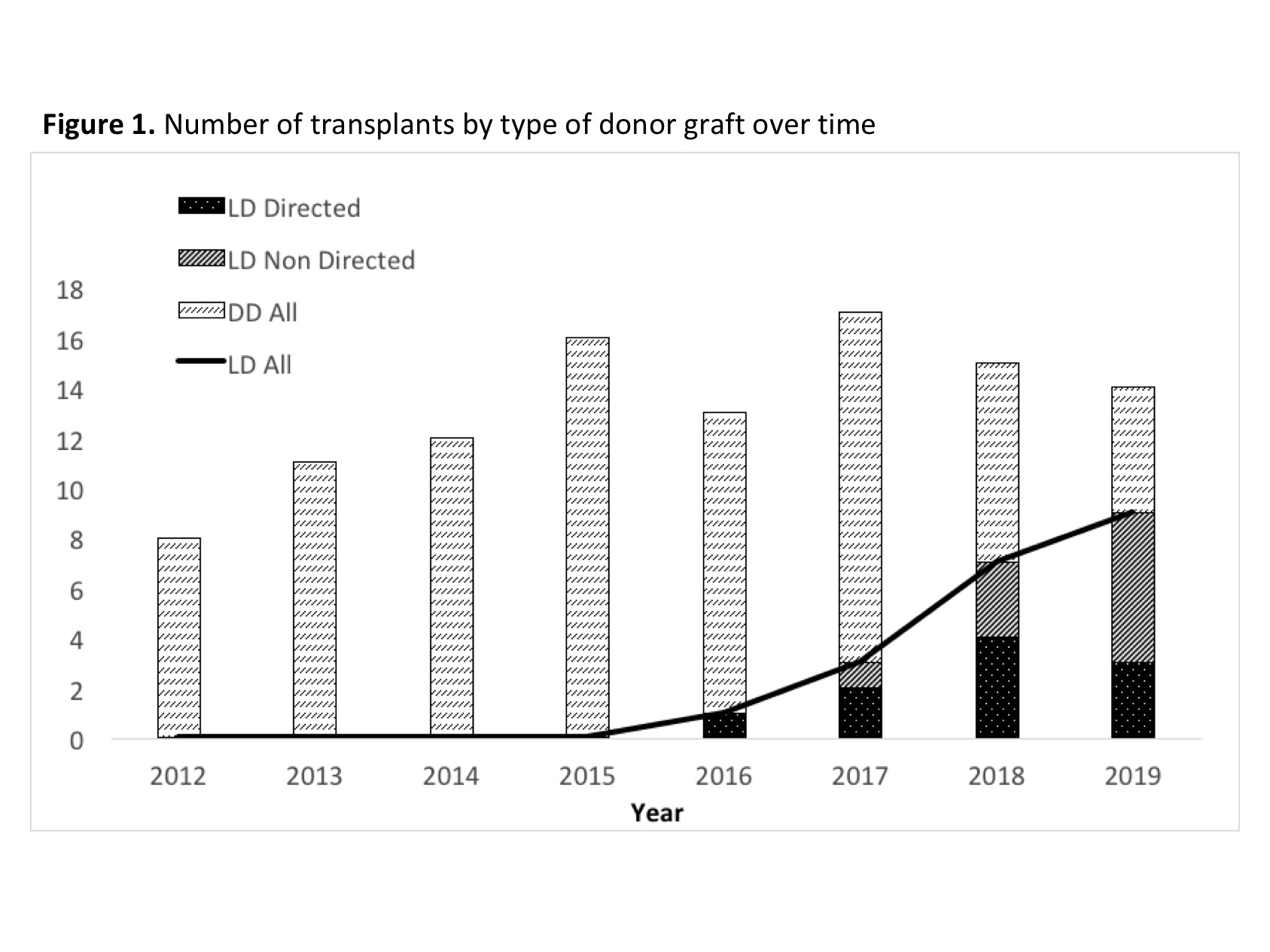
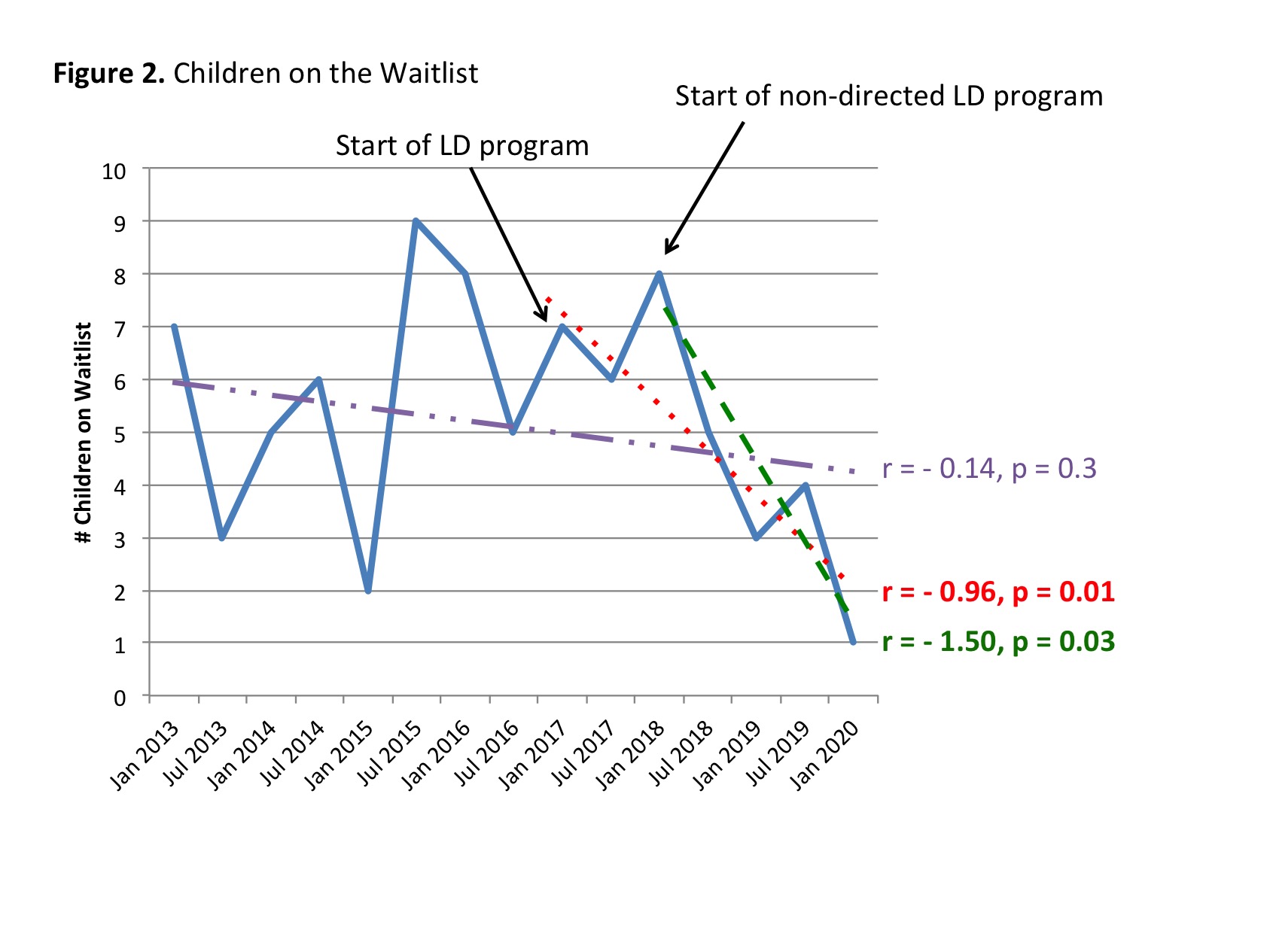
*Results: 109 pediatric candidates were listed during the study period: 6 (6%) children died or became too sick for transplant (4 (7% of 61) before and 2 (4% of 48) after the initiation of the LD program (p = 0.6)), 95 were transplanted (87%), 7 recovered and were delisted (6%), 1 remains active on the waitlist. A majority of the transplants were from deceased donors (DD) (75/95, 79%) and 20 from LD (20/95, 21%; 13 left lateral segment, 5 left lobe, 2 right lobe) (Figure 1). Ten (50%) of the LD transplants were from non-directed donors, which were allocated based on blood type, size compatibility and candidate urgency. Time on the waitlist was not significantly different by type of donor graft, even after excluding 24 recipients listed with status 1 exception (DD 73 [5 – 589] vs. LD 80 [12 – 321] days, p = 0.8). Fewer LD recipients waited > 120 days (17% vs. 30%, p = 0.3). The number of children on the waitlist significantly decreased after initiation of the LD program (Figure 2) (r = -0.96, p=0.01), with a precipitous drop observed with the introduction of non-directed donors (r = -1.5, p = 0.03). Type of donor graft did not significantly influence recipient or graft survival over a median time of 283 days for LD recipients and 1128 days for DD recipients (log-rank p = 0.8 and 0.5, respectively).
*Conclusions: The initiation of a LD liver transplant program enriched with non-directed anonymous donors has essentially eliminated our pediatric waitlist. This has impacted the balance of supply and demand at our single pediatric transplant center.
To cite this abstract in AMA style:
Yoeli D, Adams MA, Wachs ME, Sundaram SS, Choudhury RA, Conzen KD, Burton JR, Pomfret EA, Jackson WE. The Impact of Non-Directed Anonymous Live Liver Donors on the Number of Children on the Waitlist at a Single Pediatric Liver Transplant Center [abstract]. Am J Transplant. 2020; 20 (suppl 3). https://atcmeetingabstracts.com/abstract/the-impact-of-non-directed-anonymous-live-liver-donors-on-the-number-of-children-on-the-waitlist-at-a-single-pediatric-liver-transplant-center/. Accessed February 16, 2026.« Back to 2020 American Transplant Congress