Renal Cell Carcinoma in Dialysis Patients: Criteria for Transplant Wait List Inclusion
1Pathology, SUNY Downstate Medical Center, Brooklyn, NY, 2Transplant Surgery, NYP/Columbia University Medical Center, New York, NY, 3Surgery, SUNY Downstate Medical Center, Brooklyn, NY, 4Pathology & Laboratory Medicine, NYP/Weill Cornell Medical Center, New York, NY
Meeting: 2019 American Transplant Congress
Abstract number: D388
Keywords: Kidney, Renal failure, Tumor recurrence, Waiting lists
Session Information
Session Name: Poster Session D: Late Breaking
Session Type: Poster Session
Date: Tuesday, June 4, 2019
Session Time: 6:00pm-7:00pm
 Presentation Time: 6:00pm-7:00pm
Presentation Time: 6:00pm-7:00pm
Location: Hall C & D
*Purpose: End-stage renal disease (ESRD) patients on long-term hemodialysis have a higher incidence of renal cell carcinoma (RCC) in their native kidneys than the general population. Using ATS guidelines, most cancer diagnoses (e.g. breast, colon, etc.) require a cancer free period before the patient is eligible for transplant. Yet, low-stage RCC with tumor < 5 cm does not, based on the now disproven belief that RCC < 5 cm do not metastasize. Histologic subtype and tumor grade are also not considered in the eligibility criteria. With recently changed rules for acquiring waiting time, this may take on greater significance. Time is now counted from the start of dialysis rather than date of listing. Long time dialysis patients, those most likely to develop RCC, are therefore among the soonest transplanted. We reviewed our 15-year history of RCC diagnoses and correlated subtype, grade and stage with clinical outcomes for both ESRD patients and sporadic tumors. Our intention was to find evidence for or against changing ATS guidelines and instituting a watch and wait period for RCC before transplant.
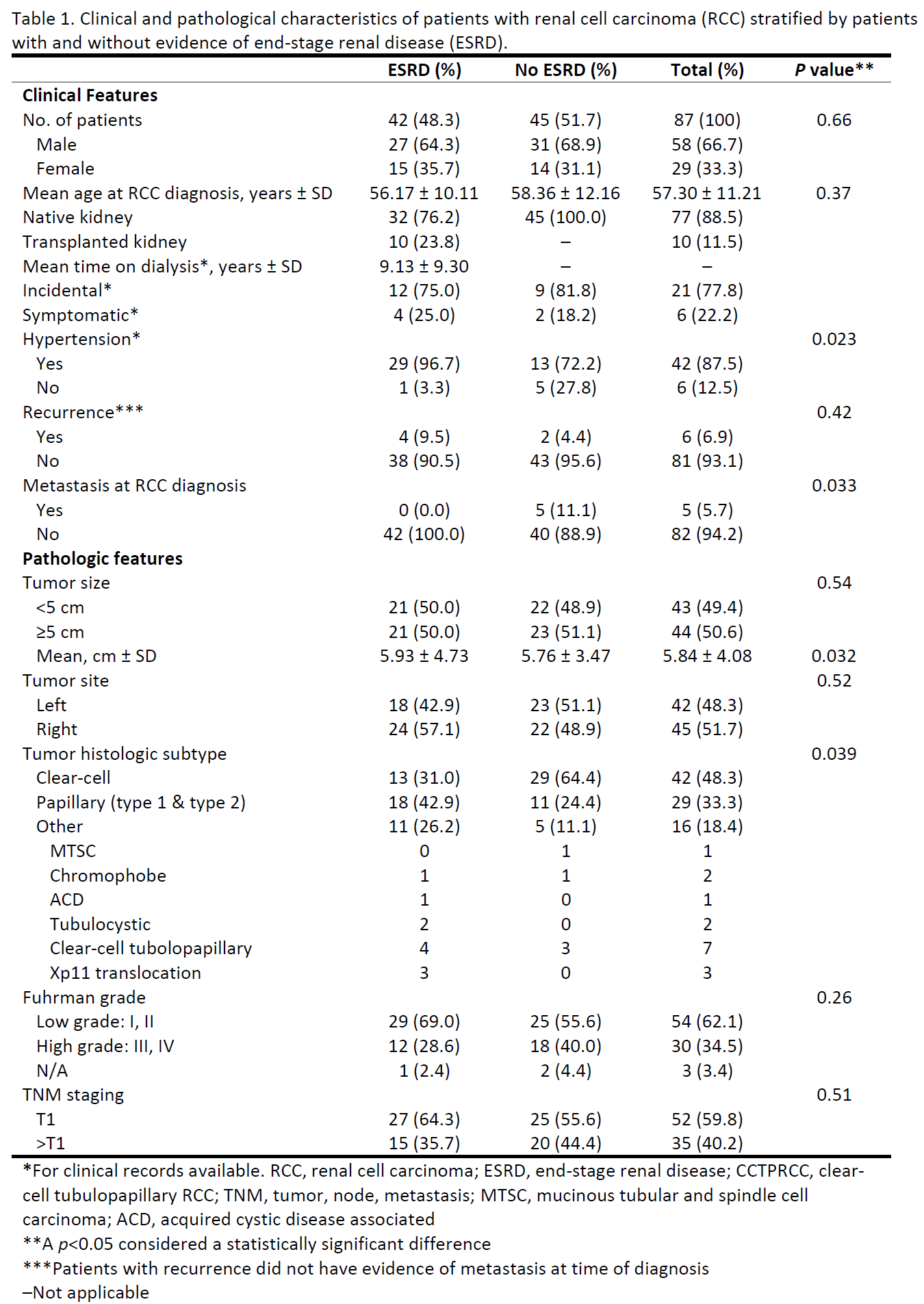
*Methods: We reviewed charts and tumor slides for all RCC diagnosed during a 15-year period (2002-2017). The pathologic characteristics assessed were: histologic subtype; tumor size; grade; and pathologic staging. The clinical data recorded were: ESRD status; renal failure cause; dialysis time; transplanted or not; immunosuppressive medication; symptomatic or incidental; treatment; and recurrence. 87 patients were identified. Analyses were based on differences between patients with and without ESRD, while correlating tumor subtype, size and grade with patient outcomes. The outcome of interest was recurrence.
*Results: There were no differences in tumor staging or grading between ESRD and non-ESRD groups (Table 1). However, further analysis showed overall recurrence was more frequent in higher grade tumors (66.7% vs. 22.2%, p=0.038). Among ESRD patients with recurrence, there was increased total time dialysis time (17.75 years vs. 6.0 years, p=0.024). In subanalysis of ESRD patients with clear-cell (CC) histology and < 5 cm tumors, recurrence was slightly more frequent compared to non-ESRD patients (33.3% vs. 0.0%, p=0.046).
*Conclusions: The CCRCC subtype should require a wait period before transplant regardless of tumor size at diagnosis.
To cite this abstract in AMA style:
Laskar DB, Zeng J, Sharma S, Jr MTSmith, Nicastri AD, Levitan D, Maglantay R, John D, Gottesman SR. Renal Cell Carcinoma in Dialysis Patients: Criteria for Transplant Wait List Inclusion [abstract]. Am J Transplant. 2019; 19 (suppl 3). https://atcmeetingabstracts.com/abstract/renal-cell-carcinoma-in-dialysis-patients-criteria-for-transplant-wait-list-inclusion/. Accessed February 2, 2026.« Back to 2019 American Transplant Congress