Willingness to Acquire Donor-Derived Hepatitis C Infection May Reduce Waitlist Mortality for Heart Transplant Candidates
NYU Langone Transplant Institute, New York, NY
Meeting: 2019 American Transplant Congress
Abstract number: D365
Keywords: Heart transplant patients, Hepatitis C, Waiting lists
Session Information
Session Name: Poster Session D: Late Breaking
Session Type: Poster Session
Date: Tuesday, June 4, 2019
Session Time: 6:00pm-7:00pm
 Presentation Time: 6:00pm-7:00pm
Presentation Time: 6:00pm-7:00pm
Location: Hall C & D
*Purpose: Hearts from deceased donors with hepatitis C infection (HCV+) are disproportionately discarded because most waitlist registrants are HCV negative (HCV-). For some with end-organ failure, the perceived risk of waitlist death outweighs fears of acquiring treatable donor-derived HCV infection. The purpose of this study was to evaluate the practice and impact of using HCV+ hearts for HCV- recipients (HCV+to- transplants).
*Methods: National data were provided by the Scientific Registry of Transplant Recipients. Odds of waitlist death were calculated using logistic regression. HCV+to- transplants were performed at the NYU Langone Transplant Institute under an IRB-approved protocol. In this study, all HCV+ donors had detectable HCV RNA by nucleic acid testing. All recipients were treated with a pan-genotypic direct-acting antiviral HCV drug.
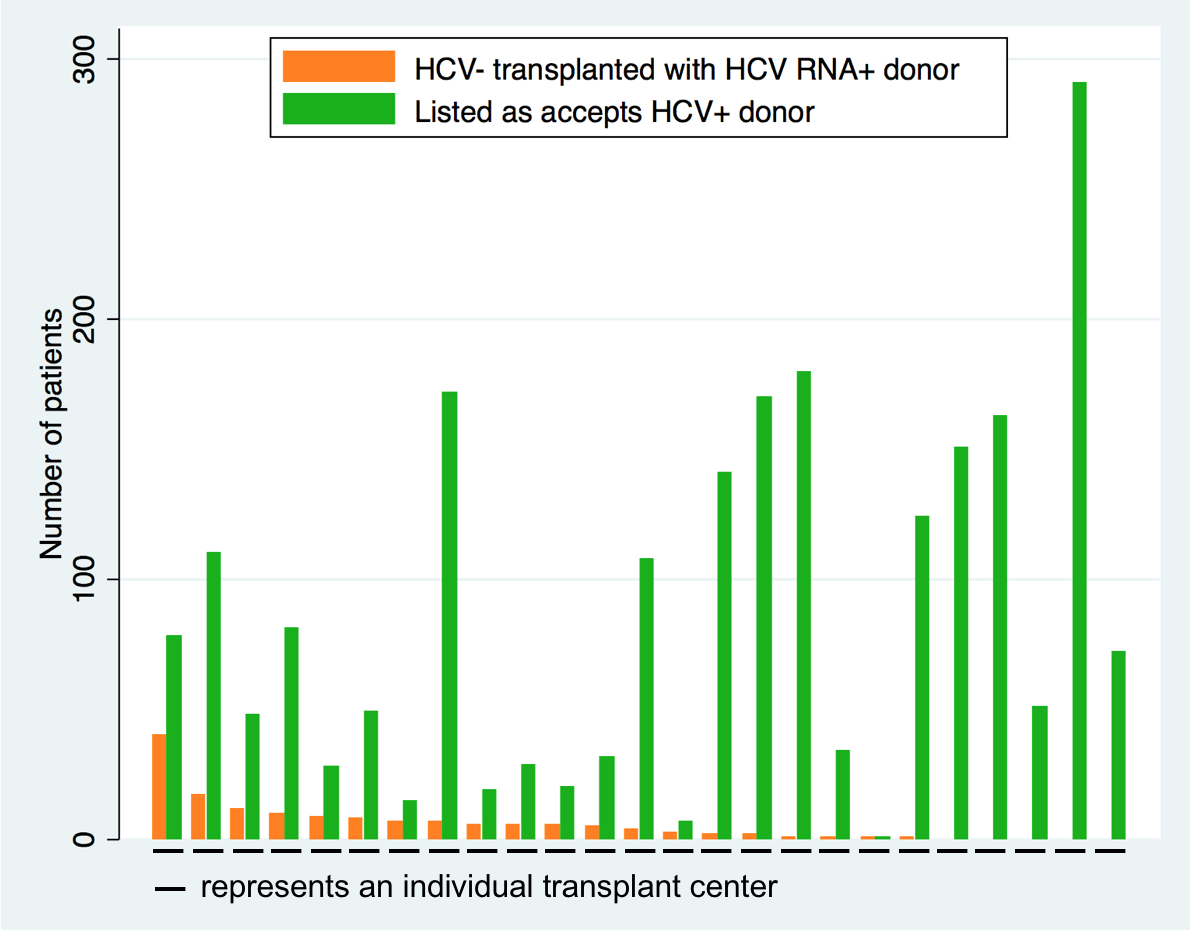
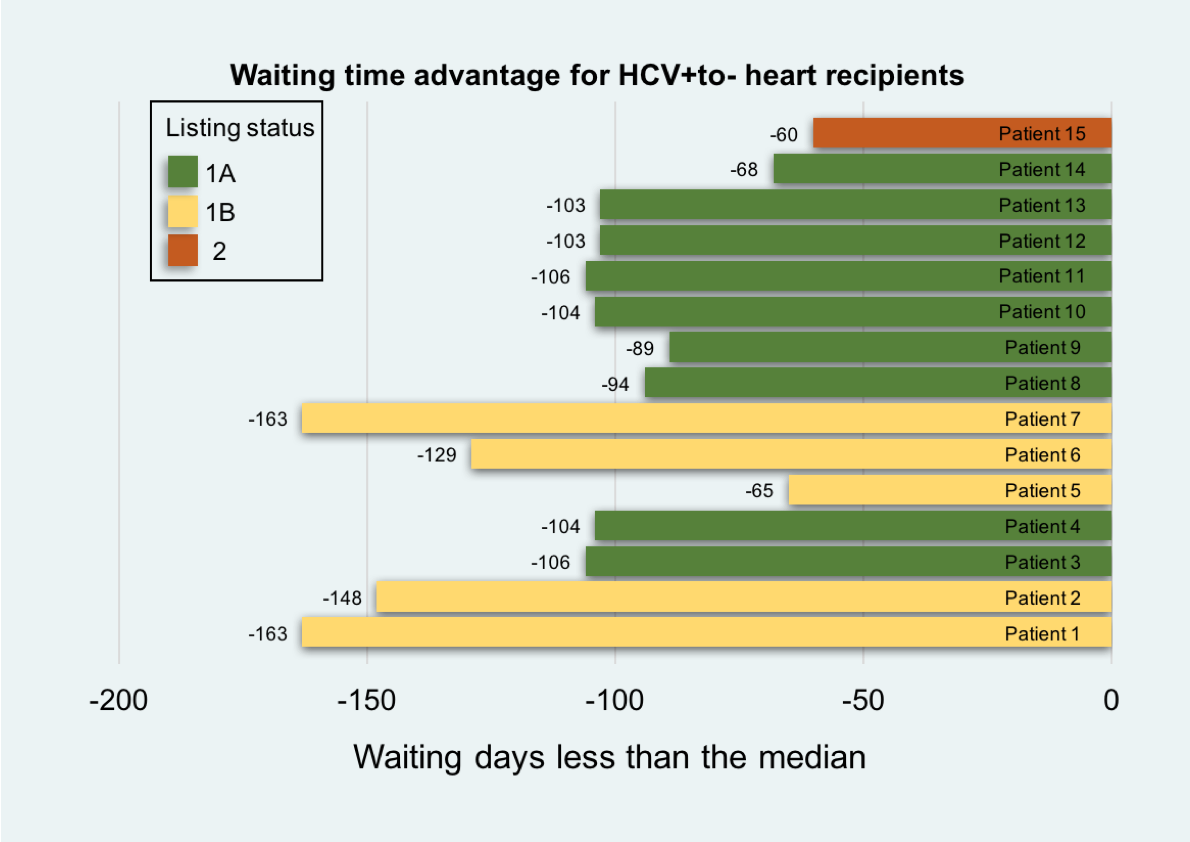
*Results: Between 2015 and 2018, the proportion of national waitlist registrants listed as accepting HCV+ hearts quadrupled (7.8% vs. 34.4%), and the incidence of HCV+to- transplants increased 10-fold (0.24% vs.2.3%). 52.7% of centers listed no HCV- candidates for HCV+ donors, 25.6% listed but performed no HCV+to- transplants, and 21.7% performed at least 1 HCV+to- transplant. Rates of listing did not correlate with rates of transplantation (Figure 1). From January through November 2018, 15 patients at NYU Langone received HCV+to- hearts and were treated for new HCV infection. Per patient, waiting time to transplant was 107±32 days less than the regional median (Figure 2). Prior to 2017, odds of waitlist death were 85% greater in our region compared to other regions (aOR=1.85; 95% CI:1.4-2.5). After implementing the HCV+to- protocol, odds of waitlist death did not differ from other regions (aOR=0.99; 95% CI:0.3-2.8).
*Conclusions: Hearts from HCV+ deceased donors may shorten waiting time to transplant and decrease waitlist mortality among HCV- patients.
To cite this abstract in AMA style:
Lonze BE, Reyentovich A, Moazami N, Smith DE, Gidea C, Montgomery RA. Willingness to Acquire Donor-Derived Hepatitis C Infection May Reduce Waitlist Mortality for Heart Transplant Candidates [abstract]. Am J Transplant. 2019; 19 (suppl 3). https://atcmeetingabstracts.com/abstract/willingness-to-acquire-donor-derived-hepatitis-c-infection-may-reduce-waitlist-mortality-for-heart-transplant-candidates/. Accessed February 15, 2026.« Back to 2019 American Transplant Congress