Specific Reasons for Public Health Service (PHS) Increased Risk (IR) Designation Had Little Influence on Doctors’ Kidney Offer Acceptance Decisions in Controlled “Lab” Experiment
1UNOS, Richmond, VA, 2CCF, Cleveland, OH, 3Duke, Durham, NC, 4Wharton, Philadelphia, PA, 5UCSD, San Diego, CA, 6Wake Forest, Winston-Salem, NC, 7Yale, New Haven, CT
Meeting: 2019 American Transplant Congress
Abstract number: D221
Keywords: Allocation, High-risk, Kidney transplantation
Session Information
Session Name: Poster Session D: Non-Organ Specific: Public Policy & Allocation
Session Type: Poster Session
Date: Tuesday, June 4, 2019
Session Time: 6:00pm-7:00pm
 Presentation Time: 6:00pm-7:00pm
Presentation Time: 6:00pm-7:00pm
Location: Hall C & D
*Purpose: Over 25% of donors are labeled as PHS “increased risk,” a designation associated with reduced organ utilization despite favorable risk/benefit calculations for most patients. OPTN data does not include specific PHS reasons, which could be collected to aid offer screening and support decision-making. We used UNOS’s DonorNet offer simulator, SimUNet, to assess the impact of PHS reasons on kidney offer acceptance decisions in a controlled experiment.
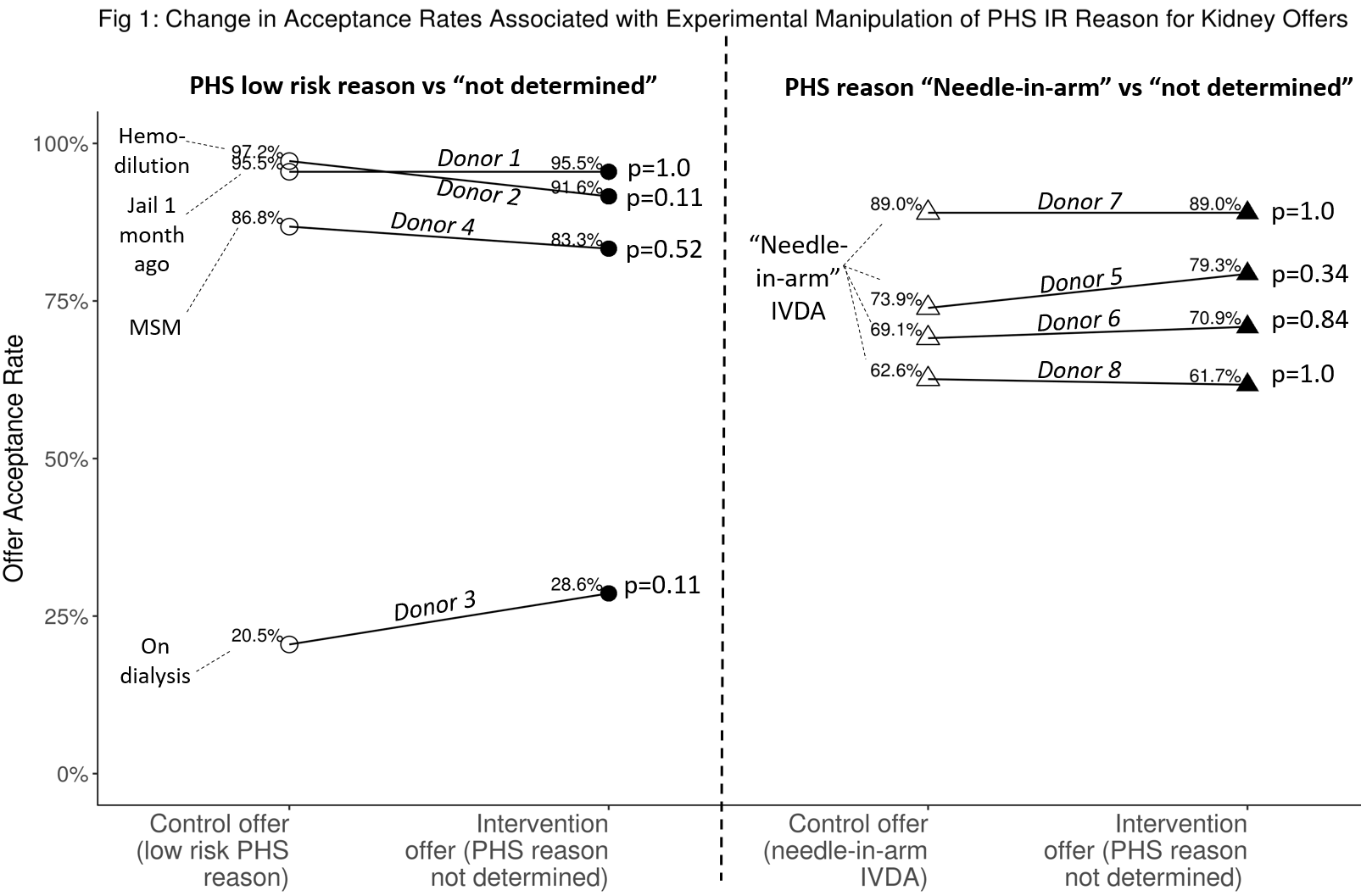
*Methods: As part of a broader study conducted 10/29-11/16/2018, 119 MDs experienced in considering kidney offers (73 surgeons, 46 physicians) each received 4 “low-risk” PHS donor offers to specific candidates (control offers), along with 4 otherwise clinically-identical offers with PHS reason “cannot be determined” to obliquely simulate absence of a reason. Low-risk reasons were hemodilution; jailed for 5 days 1 month ago; on dialysis; men who have sex w/ men (MSM). We also included 4 “needle in the arm” (NIA), intravenous drug abuse (IVDA) donors, each paired with an otherwise clinically-identical offer with reason “cannot be determined.” A crossover design with repeated measures and a minimum washout period of a weekend was used, along with clustered data analysis. We hypothesized that low risk reasons would be associated with increased acceptance and NIA with reduced acceptance.
*Results: 85% of the time, the offer acceptance decision was the same for both offer variants: control (low-risk PHS reason) and intervention (PHS reason “cannot be determined”). Altered decisions were equally likely to switch to acceptance or refusal (p=1.0, McNemar’s test). For NIA donors, 79% of the time the decision was the same. When different, the NIA variant was only slightly more likely to be declined (OR=1.17, p=0.53) than the “cannot be determined” variant. Acceptance rates were not statistically different for any of the 8 donors (Fig 1).
*Conclusions: In a lab environment, the decision to accept a kidney offer was not influenced by PHS reasons nearly to the degree hypothesized. Lower utilization of PHS IR organs might be attributable to patients’ reluctance to accept the small risk of disease transmission in the context of needing a transplant. Patients not consenting to receive PHS IR organs may contribute more toward lower organ utilization than clinician acceptance practices.
To cite this abstract in AMA style:
Stewart D, Rosendale J, McGehee H, Schold J, Lindemans J, Kessler J, Sullivan C, Mekeel K, Stratta R, Formica R, Klassen D. Specific Reasons for Public Health Service (PHS) Increased Risk (IR) Designation Had Little Influence on Doctors’ Kidney Offer Acceptance Decisions in Controlled “Lab” Experiment [abstract]. Am J Transplant. 2019; 19 (suppl 3). https://atcmeetingabstracts.com/abstract/specific-reasons-for-public-health-service-phs-increased-risk-ir-designation-had-little-influence-on-doctors-kidney-offer-acceptance-decisions-in-controlled-lab-experime/. Accessed February 6, 2026.« Back to 2019 American Transplant Congress