The Impact of Share 35 on Living Donor Liver Transplant Utilization in the United States: Analysis of UNOS Data
University of California, San Francisco, San Francisco, CA
Meeting: 2019 American Transplant Congress
Abstract number: C300
Keywords: Allocation
Session Information
Session Name: Poster Session C: Liver: MELD, Allocation and Donor Issues (DCD/ECD)
Session Type: Poster Session
Date: Monday, June 3, 2019
Session Time: 6:00pm-7:00pm
 Presentation Time: 6:00pm-7:00pm
Presentation Time: 6:00pm-7:00pm
Location: Hall C & D
*Purpose: In 2013, the Share 35 policy was implemented in the United States (US) to improve timely organ allocation to high MELD patients awaiting liver transplantation (LT). Living donor liver transplantation (LDLT) utilization in the US is highest in high MELD regions, however the median MELD at transplant for LDLT is 15. Therefore, patients awaiting LT with the potential for LDLT were unlikely to benefit from Share 35. The purpose of this study was to investigate the impact of Share 35 on LDLT utilization. We hypothesized that LDLT would increase after Share 35 to offset the shift in allocation of deceased donor livers to higher MELD patients.
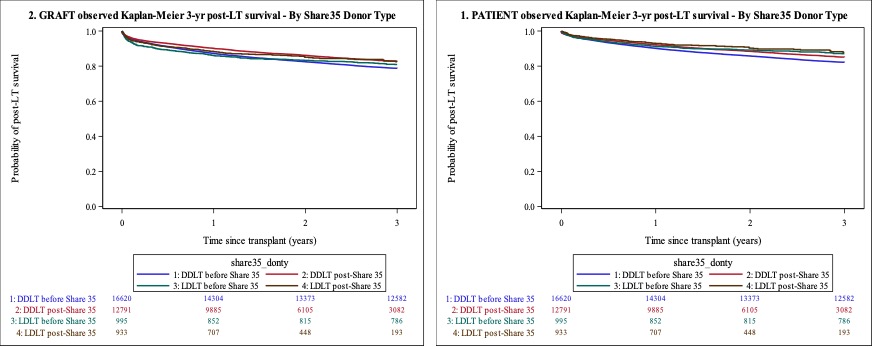
*Methods: United Network for Organ Sharing (UNOS) data from 2008-2018 was utilized, with 2008-2013 classified as the pre-Share 35 era, and 2013-2018 classified as post-Share 35. Among the two eras, we compared demographic data using Wilcoxon rank sum and chi-squared tests; graft and patient survival were estimated using Kaplan-Meier methods.
*Results: 52,225 primary adult single-organ liver transplants for non-fulminant liver disease occurred during the study period, with 25,701 occurring pre-Share 35 (24,701 deceased donors, 995 LDLT) and 26,524 post-Share 35 (24,706 deceased donors, 1215 LDLT). The percent of LDLT of total liver transplant volume increased significantly (4.6% post vs. 3.9% pre, p<0.001). Among the LDLT patients in pre and post eras, there was no significant difference in the median MELD at transplant (16 IQR 13-22 vs. 16 IQR 11-22, p=0.07), gender distribution (42.9% vs. 44.1% female), or BMI (26 vs. 26.4). Compared with the pre era, the post era had older patients (57 vs. 55 years, p<0.001, more Hispanic patients (12.8% vs. 8.9%, p=0.03), fewer patients with HCV (20.7% vs. 30.3%, p<0.001), and more patients with public insurance (30.3% vs. 24.7%, p=0.004). LDLT utilization varied significantly by region (p<0.001). Regions 2, 4, 5, 8, 10 all demonstrated significant increases in LDLT utilization post-share 35; the deceased donor median MELD at transplant also increased significantly in regions 2 (25 IQR 22-33 vs. 29 IQR 25-34, p=0.01), 4 (27 IQR 23-31 vs. 29 IQR 25-35, p<0.001), and 5 (31 IQR 27-37 vs. 34 IQR 29-39, p=0.003) after the implementation of Share 35.
Among the two eras, there was a significant improvement in graft survival among DDLT recipients at both one and three years after transplant (90.1% vs. 87.2% and 82.7% vs. 78.7%, respectively, p-values<0.001) and in patient survival at one and three years after transplant (92.2 vs. 90.1% and 85.1% vs. 82.2%, p-values <0.001). There was no significant difference in graft or patient survival for LDLT recipients pre versus post-Share 35 (Figure 1).
*Conclusions: LDLT utilization in the United States increased significantly following the implementation of Share 35. This trend varied by region and is likely multifactorial, owing to a combination of increased patient demand as well as center experience. DDLT outcomes post- Share 35 improved and there was no change in LDLT outcomes, suggesting that Share 35 is not compromising survival in either population.
To cite this abstract in AMA style:
Braun HJ, Dodge JL, Grab JD, Hirose R, Stock PG, Ascher NL. The Impact of Share 35 on Living Donor Liver Transplant Utilization in the United States: Analysis of UNOS Data [abstract]. Am J Transplant. 2019; 19 (suppl 3). https://atcmeetingabstracts.com/abstract/the-impact-of-share-35-on-living-donor-liver-transplant-utilization-in-the-united-states-analysis-of-unos-data/. Accessed February 22, 2026.« Back to 2019 American Transplant Congress