Predicting Graft Loss in a Population of Kidney Transplant Patients Diagnosed With ABMR/TG
1Laboratory Medicine and Pathology, University of Alberta, Edmonton, AB, Canada
2Medicine, University of Alberta, Edmonton, AB, Canada.
Meeting: 2015 American Transplant Congress
Abstract number: 179
Keywords: Kidney transplantation, Rejection, Survival
Session Information
Session Name: Concurrent Session: Immune Monitoring I
Session Type: Concurrent Session
Date: Monday, May 4, 2015
Session Time: 2:15pm-3:45pm
 Presentation Time: 2:27pm-2:39pm
Presentation Time: 2:27pm-2:39pm
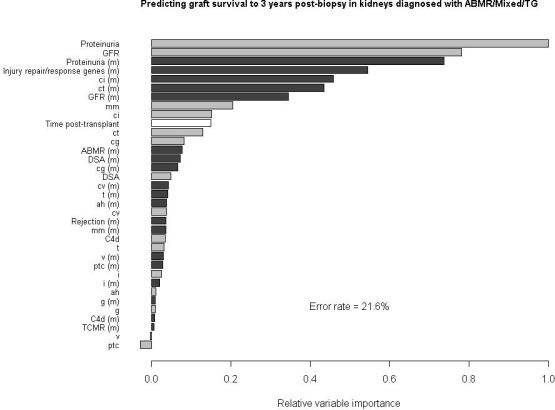
Location: Room 120-ABC
ABMR is the main cause of late graft loss in kidney transplants. Our goal was to determine the variables most strongly predictive of graft loss within three years of a biopsy for cause, in patients that had been diagnosed with either ABMR, transplant glomerulopathy (TG), or mixed (ABMR/TCMR) rejection. A number of histo-clinical variables were used, including lesion scores, GFR, presence/absence of proteinuria, DSA, C4d staining, and time post-transplant. In addition, molecular classifier scores for all of the above histo-clinical variables were included, as were IRRAT (injury repair and response genes) scores and scores from our previously published TCMR, ABMR, and rejection classifiers. Predictions were made using a random forest classifier, and predictive accuracy was assessed using Harrell's C-statistic. Figure 1 shows the relative importance of all the predictive variables used. An (m) after the variable name indicates a molecular predictor. Relative importance was assessed by permuting the values of each variable in turn, and measuring the decline in predictive accuracy in the test sets. The most important variables are those whose randomization results in the greatest loss of accuracy. The error rate shown here (21.6%) was that obtained using all diagnostic groups in the training sets, and is slightly better than that obtained if only ABMR/TG biopsies are used to train (23.5%).
The most important variables predicting outcome are all measures of tissue damage, including proteinuria, GFR, fibrosis, and their molecular classifier equivalents. Of note is the fact that the variables used in the diagnosis of ABMR (g, ptc, cg, DSA, C4d) as well as v lesions are all relatively unimportant in assessing risk of failure. Thus the variables that establish the diagnosis of ABMR are not the same as those that predict progression to failure in ABMR. To a large extent, the relative importance for predicting graft loss in ABMR mirrors that in the overall population of unselected biopsies. Knowing the diagnosis does not improve risk prediction if the molecular and histo-clinical correlates of tissue damage are available.
To cite this abstract in AMA style:
Reeve J, Halloran P. Predicting Graft Loss in a Population of Kidney Transplant Patients Diagnosed With ABMR/TG [abstract]. Am J Transplant. 2015; 15 (suppl 3). https://atcmeetingabstracts.com/abstract/predicting-graft-loss-in-a-population-of-kidney-transplant-patients-diagnosed-with-abmrtg/. Accessed February 16, 2026.« Back to 2015 American Transplant Congress
