Early Allograft Dysfunction Does Not Predict Graft or Patient Survival in Recipients of Living Donor Liver Transplantation
University of California, San Francisco, San Francisco, CA
Meeting: 2019 American Transplant Congress
Abstract number: B347
Keywords: Liver grafts, Outcome
Session Information
Session Name: Poster Session B: Liver: Living Donors and Partial Grafts
Session Type: Poster Session
Date: Sunday, June 2, 2019
Session Time: 6:00pm-7:00pm
 Presentation Time: 6:00pm-7:00pm
Presentation Time: 6:00pm-7:00pm
Location: Hall C & D
*Purpose: The rationale for left lobe utilization in living donor liver transplantation (LDLT) is that removal of a smaller liver segment that is still sufficient for the recipient leaves greater residual liver volume in the donor, and thereby decreases donor risk. Smaller graft size, however, has been associated with adverse short and long term outcomes in LDLT recipients. It has been reported that early allograft dysfunction (EAD), defined as INR>1.6 on post-operative day (POD) 7, tbili>10 on POD7, or transaminases > 2000 within the first seven days after transplant, is associated with smaller graft size as well as inferior recipient outcomes after LDLT. The purpose of this study was two-fold: 1) to determine whether a difference in the predicted and actual volumes of donated liver segments predicted EAD, and 2) to evaluate whether EAD predicted graft and patient survival in recipients of LDLT.
*Methods: We conducted a retrospective review of LDLT donors and recipients at our United States institution between 2003-2016. Demographic, clinical, and laboratory data were collected. Statistical analyses were performed using Wilcoxon rank sum, chi-squared tests, and regression modeling; graft and patient survival were estimated using Kaplan-Meier methods.
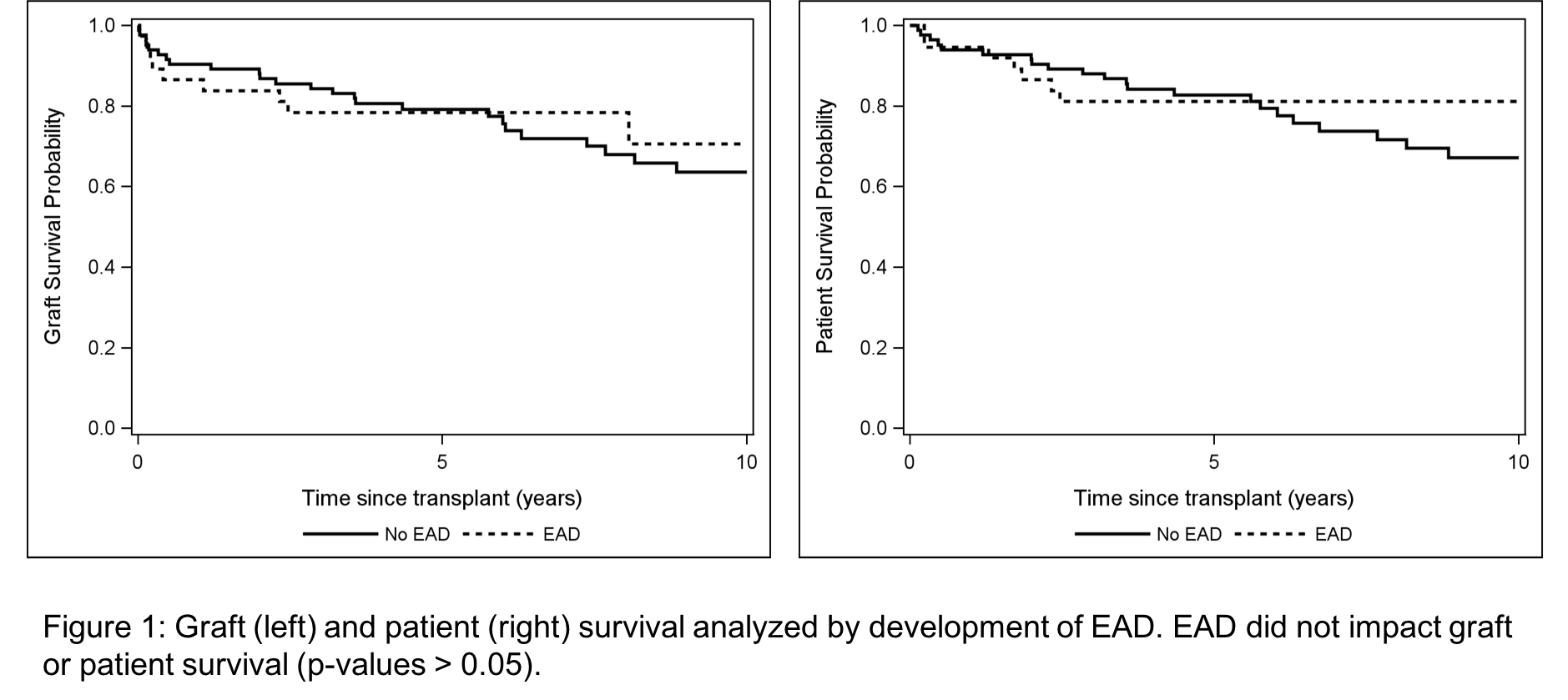
*Results: Between 2003-2016, 136 patients underwent LDLT; 123 are included in this analysis with full laboratory data. Recipients were predominantly female (54.5%), related to their donor (71.0%), transplanted for a diagnosis of HCV (34.1%), and received a left lobe graft (51.2%). Among all recipients, the median predicted graft volume was 755 cm3, the median actual graft volume was 600 cm3, and the median actual:predicted ratio was 0.78. Thirty seven (30.8%) of patients developed EAD. Patients with EAD were more often recipients of a left lobe, but there were no other significant clinical or demographic differences. In univariate and multivariable analyses, actual versus predicted graft volume did not predict development of EAD. Furthermore, there was no significant difference in graft or patient survival when outcomes were stratified by EAD (Figure 1).
*Conclusions: EAD was defined and validated using data from recipients of deceased donor liver transplants and correlates with graft and patient survival in these populations. In the LDLT population, however, there have been mixed results, with some studies suggesting EAD impacts outcomes, and other demonstrating no impact of EAD on LDLT recipients. Our findings demonstrate that EAD occurs more frequently in recipients of left lobes, but that this does not adversely impact graft or patient survival.
To cite this abstract in AMA style:
Braun HJ, Dodge JL, Grab JD, Ascher NL, Roberts JP. Early Allograft Dysfunction Does Not Predict Graft or Patient Survival in Recipients of Living Donor Liver Transplantation [abstract]. Am J Transplant. 2019; 19 (suppl 3). https://atcmeetingabstracts.com/abstract/early-allograft-dysfunction-does-not-predict-graft-or-patient-survival-in-recipients-of-living-donor-liver-transplantation/. Accessed February 7, 2026.« Back to 2019 American Transplant Congress