Overcoming Anti-HLA Sensitization in Kidney Transplantation
1Nephrology Post-Graduation, University of Sao Paulo, São Paulo, Brazil, 2Kidney Transplant Unit, Hospital Samaritano de São Paulo, São Paulo, Brazil
Meeting: 2019 American Transplant Congress
Abstract number: B186
Keywords: Alloantibodies, Highly-sensitized, Panel reactive antibodies, Survival
Session Information
Session Name: Poster Session B: Kidney Immunosuppression: Desensitization
Session Type: Poster Session
Date: Sunday, June 2, 2019
Session Time: 6:00pm-7:00pm
 Presentation Time: 6:00pm-7:00pm
Presentation Time: 6:00pm-7:00pm
Location: Hall C & D
*Purpose: To evaluate if it is possible to achieve good results in kidney transplantation (Ktx) regardless the degree of anti-HLA sensitization.
*Methods: 143 adult living (LD) and 104 deceased (DD) KTx performed between Jan/08 and Dec/16, were retrospectively divided in 3 groups: PRA=0, PRA≠0 without A, B, DR-DSA and PRA≠0 with A, B, DR-DSA. When sensitized, patients were cleared for surgery after a T and B-cell FCXM when receiving a LD and after T and B-cell CDC-XM when receiving a DD kidney. Patients with PRA=0, were induced with 40 mg of anti-IL2R, and those with PRA≠0 received 6mg/kg of anti-thymocyte globulin. IVIG 2g/kg were associated at POD 1, 21 and 42, when DSA was present. Sensitized patients repeated PRA and performed a protocol biopsy on POD 7. ABMR episodes were treated with apheresis, anti-CD20 and IVIG. Baseline characteristics of the patients are presented in the table 1.
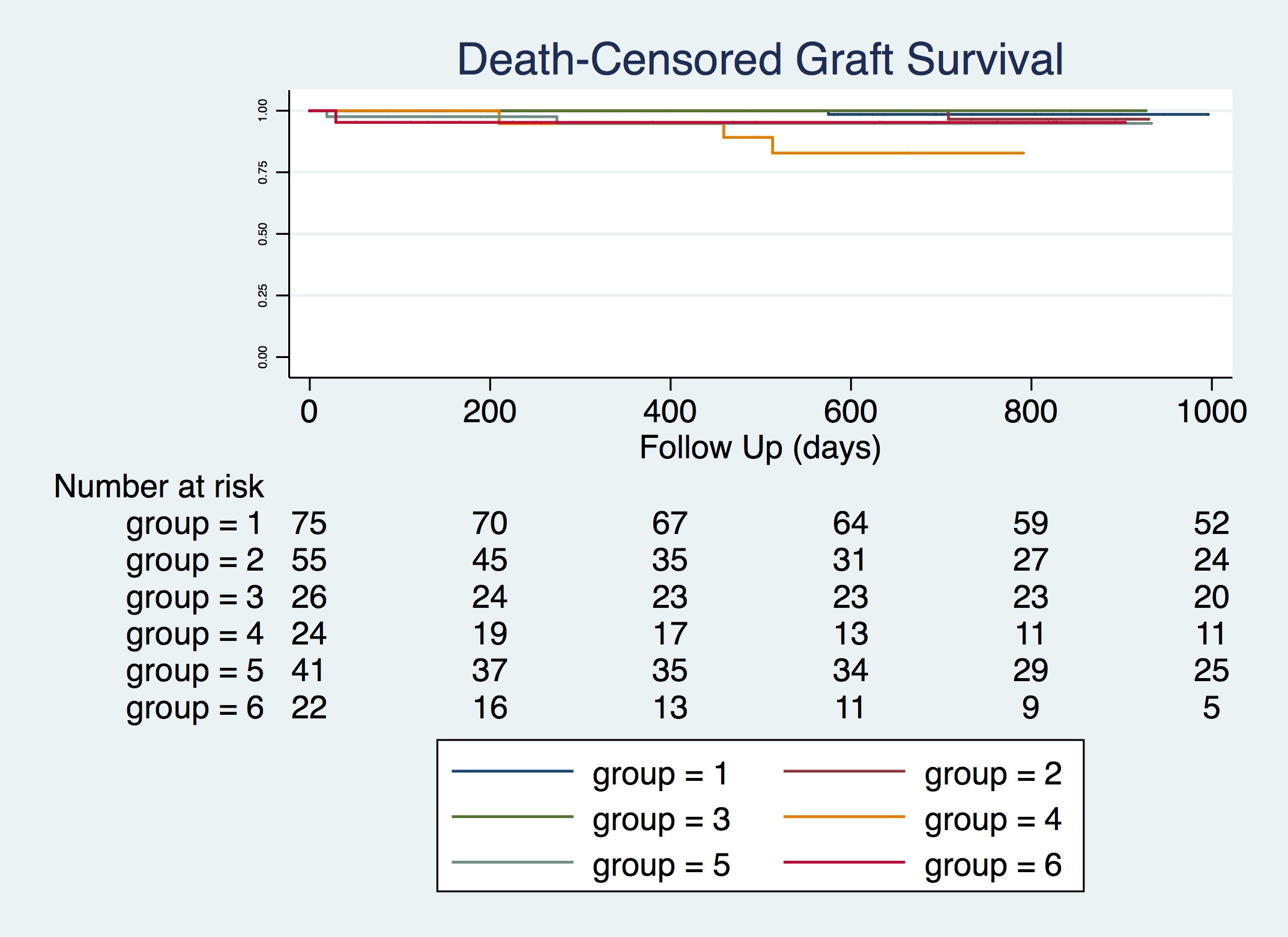
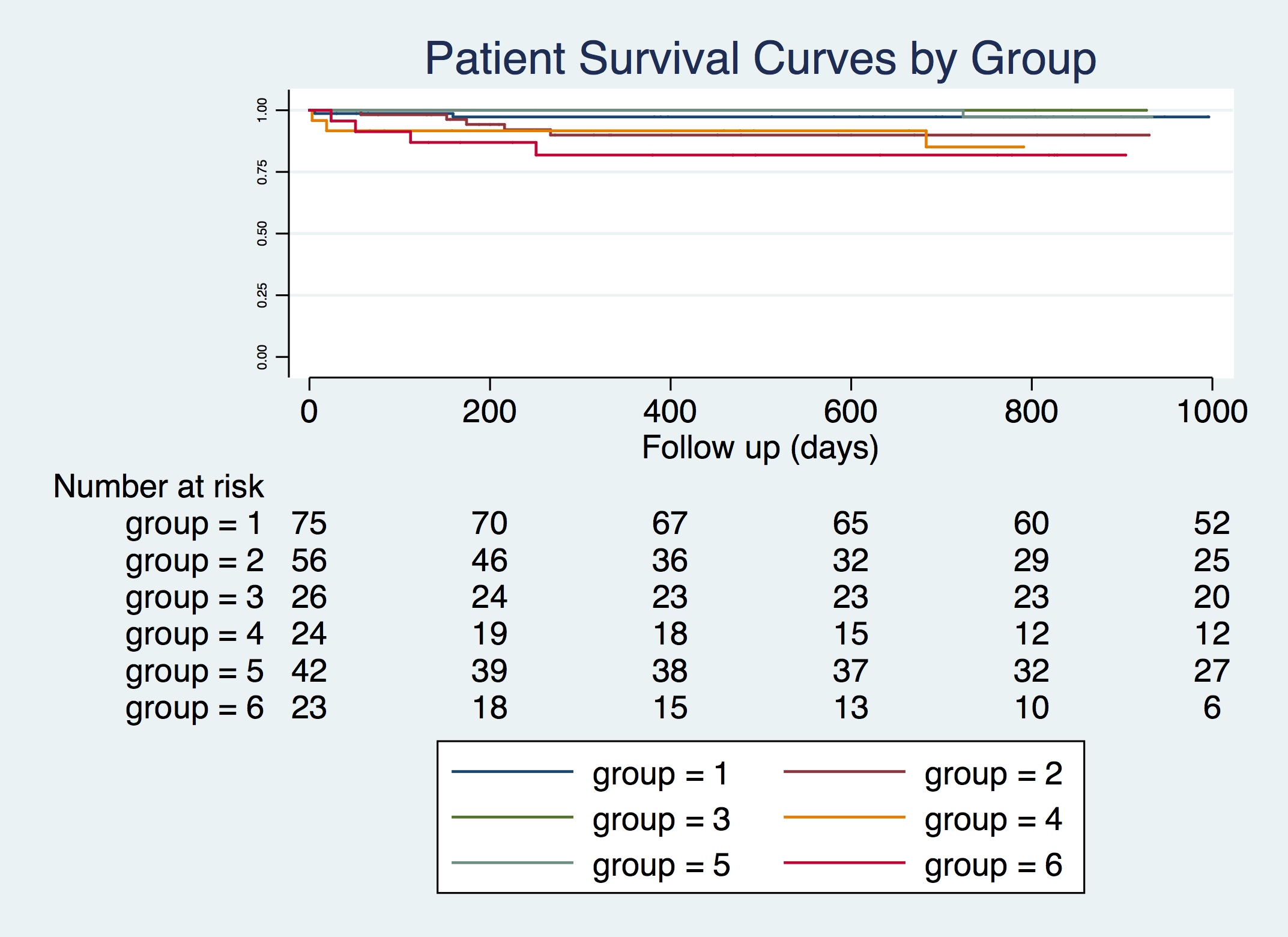
*Results: We detected differences on the overall rate of ABMR between groups 1,2 (PRA=0) and groups 3,4,5,6 (PRA≠0): 1.54% vs. 18,8%, p<0.001. Groups 5,6 (with DSA) presented more ABMR episodes than groups 1,2,3,4 (no DSA): 30.30% vs. 2.21%, p<0.001. Overall 3y LD (groups 1,3,5) and DD (groups 2,4,6) patient (0.98, 95%IC 0.93-0.99 vs 0.87, 95%IC 0.78-0.92, p=0.001) and graft survival were different (0.98, 95%IC 0.93-0.99 vs 0.90, 95%IC 0.79-0.96, p=0.002). Although the higher frequency of ABMR in positive DSA patients (5,6), no differences at 3 y patient and death-censored graft survival could be observed related to anti-HLA sensitization in LD (1,3,5): 0.97 vs 1.00 vs 0.97, p=0.93; 0.98 vs 1.00 vs 0.95, p=0.05 and in DD (2,4,6): 0.90 vs 0.85 vs 0.81, p=0.56; 0.92 vs 0.83 vs 0.95, p=0.25, as can be seen in the graphics bellow.
*Conclusions: Good results on patient and graft survival of highly-sensitized patients can be achieved knowing the individual immunological risks, adapting induction therapies and improving diagnostic and treatment methods for ABMR.
To cite this abstract in AMA style:
Siqueira RC, Malafronte P, Baptista-Silva JC, Silva EF, Camargo MC, Castro MCRibeiro. Overcoming Anti-HLA Sensitization in Kidney Transplantation [abstract]. Am J Transplant. 2019; 19 (suppl 3). https://atcmeetingabstracts.com/abstract/overcoming-anti-hla-sensitization-in-kidney-transplantation/. Accessed February 15, 2026.« Back to 2019 American Transplant Congress