Patterns Of Anti-retroviral Use Among U.s. Liver Transplant Candidates With Hiv
1Johns Hopkins University, Baltimore, MD, 2Epidemiology, University of North Carolina, Chapel Hill, NC, 3Surgery & Epidemiology, Johns Hopkins University, Baltimore, MD
Meeting: 2019 American Transplant Congress
Abstract number: A352
Keywords: African-American, HIV virus, Liver failure, Public policy
Session Information
Session Name: Poster Session A: Transplant Infectious Diseases
Session Type: Poster Session
Date: Saturday, June 1, 2019
Session Time: 5:30pm-7:30pm
 Presentation Time: 5:30pm-7:30pm
Presentation Time: 5:30pm-7:30pm
Location: Hall C & D
*Purpose: There is a high burden of liver disease among HIV-infected (HIV+) individuals, and the class of antiretroviral therapy (ART) used for their treatment may complicate post-transplant immunosuppression management. It is, therefore critical to understand which regimens are commonly used in this population and how this has changed over time.Therefore, we sought to estimate the prevalence HIV among US liver transplant candidates and describe trends in ART use.
*Methods: We linked pharmacy claims data to the national transplant registry (2007-2016), and identified HIV+ candidates by fills of ART prescription medications exclusive to HIV treatment. After exploring potential mechanism(s) of missingness, we estimated HIV prevalence using multiple imputation by chained equations (MICE). We then explored factors associated with ART regimens using logistic regression.
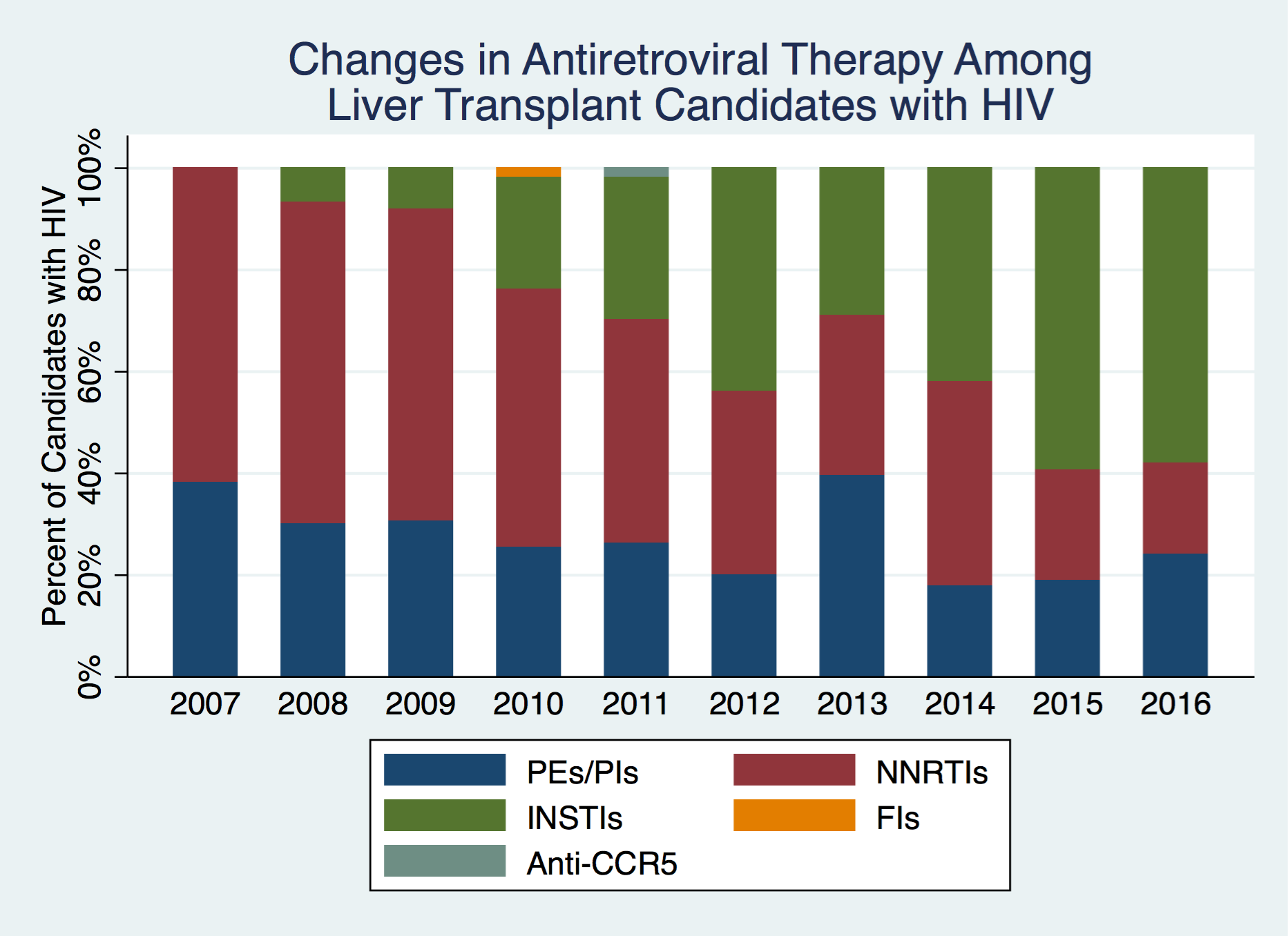
*Results: The pharmacy data linkage contained 91.0% (n=99,376) of all candidates in the national transplant registry in the study period. We identified 857 HIV+ candidates with an overall estimated prevalence of 0.95% (95% Confidence Interval: 0.89%-1.02%). HIV+ candidates were more often young (median [IQR]: 53 [48-59] vs. 56 [50-62]), African American (21.4 vs. 9.0%), and male (80.6 vs. 64.4%), with liver disease due to hepatitis C virus (33.5 vs. 26.1%) than HIV- candidates (p<0.001 for all). We found a distinct shift in the ART regimens over time (Figure 1).
The use of pharmacoenhancers (PI/PEs) decreased over time (48.4% in 2007 to 20.0% in 2016) and were more likely to be used by African American candidates (aOR: 1.80, 95%CI: 1.18-2.74, p<0.01), adjusting for age, year, and sex. Conversely, integrase inhibitor (INSTI) use increased over time (7.8% in 2008 to 52.3% in 2016) and was not associated with race (aOR: 1.02, 95% CI:0.62-1.64, p=.95) adjusting for age, year, and sex.
*Conclusions: We used a novel data linkage to identify a unique and previously unstudied population of HIV+ liver transplant candidates on the US waitlist. We found that the burden of HIV on the liver transplant waitlist was nearly 1%, ART use has shifted over time, and African Americans were almost twice as likely to be prescribed ART regimens containing pharmacoenhancers, which can interact with post-transplant immunosuppression.
To cite this abstract in AMA style:
Shaffer AA, Thomas AG, Segev DL. Patterns Of Anti-retroviral Use Among U.s. Liver Transplant Candidates With Hiv [abstract]. Am J Transplant. 2019; 19 (suppl 3). https://atcmeetingabstracts.com/abstract/patterns-of-anti-retroviral-use-among-u-s-liver-transplant-candidates-with-hiv/. Accessed February 16, 2026.« Back to 2019 American Transplant Congress