Early Renal Allograft Failure after Simultaneous Liver-Kidney Transplantation: Evidence for Utilization of the Safety Net
1UCSF, San Francisco, CA, 2Columbia University, New York, NY, 3University of Alabama at Birmingham, Birmingham, AL
Meeting: 2019 American Transplant Congress
Abstract number: A276
Keywords: Kidney/liver transplantation, Liver cirrhosis, Renal dysfunction, Renal failure
Session Information
Session Name: Poster Session A: Liver - Kidney Issues in Liver Transplantation
Session Type: Poster Session
Date: Saturday, June 1, 2019
Session Time: 5:30pm-7:30pm
 Presentation Time: 5:30pm-7:30pm
Presentation Time: 5:30pm-7:30pm
Location: Hall C & D
*Purpose: Utilization of simultaneous liver-kidney transplant (SLKT) has increased dramatically during the Model for End-Stage Liver Disease (MELD) era. Prior studies have demonstrated a modest benefit of SLKT over kidney after liver transplant (KALT) on overallsurvival, but little is known of the impact of SLKT on kidney graft function. We aimed to determine the impact of SLKT, as compared to KALT, on early renal allograft failure (RF).
*Methods: UNOS data for all adult patients (≥18) who received either a SLKT or KALT from 2002-2017 were analyzed. The primary outcome was 90d-RF (as reported to UNOS, at 90 days post-renal transplant). Secondary outcome was 1y-RF. We compared the following groups of patients: SLKT<25 (SLKT with end MELD<25), SLKT25/35 (end MELD ≥25/<35), and SLKT35 (end MELD≥35) to KALT. We generated a propensity-score (PS) using logistic regression for receiving either a SLKT or KALT using the following variables: age, cirrhosis etiology, MELD at LT, time on hemodialysis, center, and list year. Cox-regression clustered on center then determined the association between the groups and both 90d-RF/1y-RF after adjusting for PS-quintiles and kidney donor profile index (KDPI). We utilized the median KDPI for each group to compare predicted with observed renal graft survival.
*Results: Of the 5991 patients included in this study: 1485 KALT, 1274 SLKT<25, 1842 SLKT25/35, 1390 SLKT≥35. Baseline characteristics differed by group (KALT, SLKT<25, SLKT25/35, SLKT≥35): median age (58v.56v.58v.56y, p<0.001); %female (34v.37v.36v.38%, p<0.001), %diabetes (48v.35v.42v.35, p<0.001), %hypertension (6v.10v.7v.5, p<0.001), median KDPI (0.5v.0.4v.0.4v.0.3, p<0.001). % of patients with 90d- and 1y-RF in KALT, SLKT<25, SLKT25/35, and SLKT≥35 groups (p<0.001, test for trend): 90d-RF: 3.3v.5.1v.7.0v.8.8%; 1y-RF: 5.1v.8.2v.11.0v.13.5%. For reference, based on median KDPI of the kidneys transplanted in each group, the expected % 1y-RF was:5.5v.5.6v.5.6v.4.2% and during the same period, DDRT recipients had 3.3% 90d-RF and 6.2% 1y-RF.
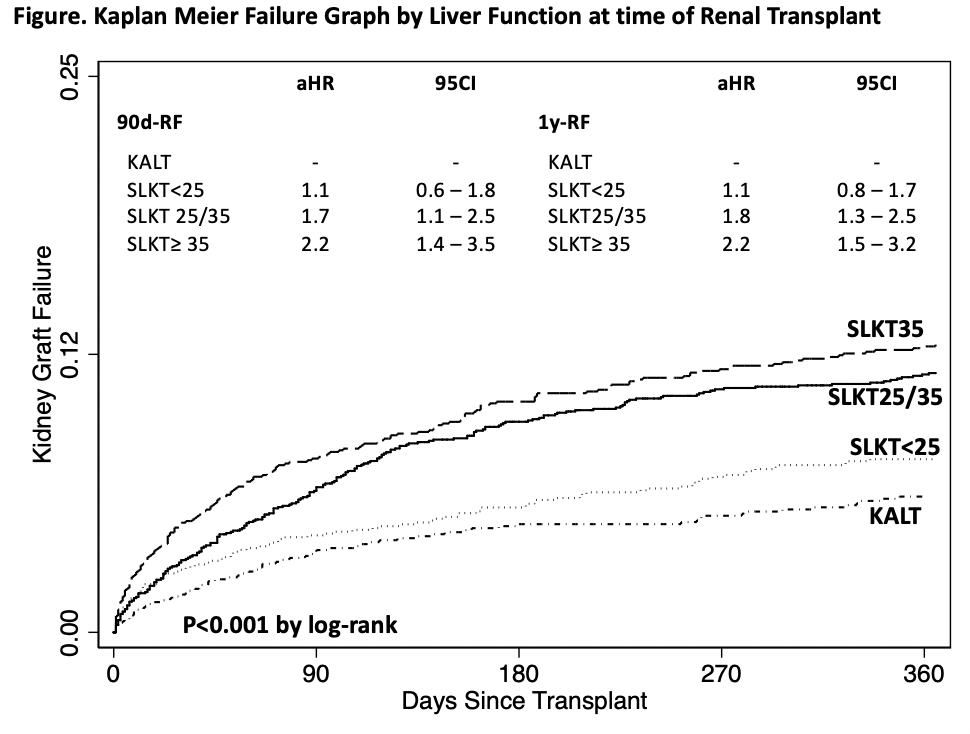
After adjusting for KDPI and PS-quintiles, compared to KALT, those undergoing SLKT had significantly higher rates of 90d- and 1y-RF: 90d-RF: SLKT<25: HR 1.1 (95CI 0.7-1.8), SLKT25/35: HR 1.7 (1.1 - 2.5), SLKT≥35 2.2 (1.4 - 3.5)1y-RF: SLKT<25: HR 1.2 (95CI 0.8-1.7), SLKT25/35: HR 1.8 (1.3 - 2.5), SLKT≥35 2.2 (1.5 - 3.2); (Figure).
*Conclusions: As compared to KALT recipients, patients undergoing SLKT with a MELD score ≥25/<35 or ≥35 had 170% and 220% the risk of 90-RF and 180% and 220% the risk of 1y-RF, respectively. Given the now well-established “safety net”, KALT may serve as an opportunity to improve renal allograft outcomes in patients with a MELD score ≥25.
To cite this abstract in AMA style:
Cullaro G, Verna EC, Orandi BJ, Lai JC. Early Renal Allograft Failure after Simultaneous Liver-Kidney Transplantation: Evidence for Utilization of the Safety Net [abstract]. Am J Transplant. 2019; 19 (suppl 3). https://atcmeetingabstracts.com/abstract/early-renal-allograft-failure-after-simultaneous-liver-kidney-transplantation-evidence-for-utilization-of-the-safety-net/. Accessed March 7, 2026.« Back to 2019 American Transplant Congress