Association of HLA Amino Acid Mismatches with Kidney Allograft Failure
U of PA, Philadelphia, PA
Arbor Res. Collaborative for Health, Ann Arbor, MI
Natl. Marrow Donor Program, Minneapolis, MN
Pathology, Stanford U, Palo Alto, CA
Internal Med., U of MI, Ann Arbor, MI
Meeting: 2013 American Transplant Congress
Abstract number: 170
The effect of HLA matching on kidney allograft survival is usually analyzed based on HLA serologic specificity and does not take into account other HLA structural differences that may significantly affect organ alloreactivity. We analyzed the effect of HLA mismatches (mm) at the amino acid (AA) level on allograft survival; this approach is an important step for the development of better strategies for donor selection, tolerance induction, and titrating immunosuppression.
Allele-level HLA haplotypes were computed by statistical inference based on haplotype frequencies stratified by race using HLA phenotypes of donors and recipients. Lists of all possible AA mm sites with the corresponding probability were created, based on a computation over the distribution of the possible alleles for each HLA-A, B, and DR specificity. This method was validated on several datasets and showed a high accuracy of the estimated AA mm at most HLA-A, B, and DR variable sites. Scientific Registry of Transplant Recipients data from 1987-2009 on 156,047 deceased-donor kidney Txp were used to test the association of graft survival with imputed AA mm sites. A Cox proportional hazards regression model of time to graft failure (GF) was fitted to estimate the effect of the imputed number of mm sites within each HLA locus, adjusting for donors and recipients characteristics including HLA-A, B, and DR antigen mm.
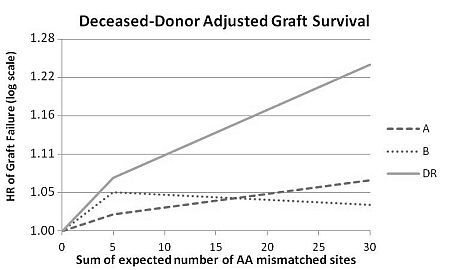
The median expected number of HLA AA mm sites was 9.4 at HLA-A (interquartile range 2.6-14.8), 9.0 at B (3.9-13.4), and 7.3 at DR (1.8-11.4). The adjusted hazard ratio (HR) of GF associated with every five additional AA mm was 1.01 for HLA-A (p = 0.02), 1.00 for HLA-B (p = 0.95), and 1.04 for HLA-DR (p<0.0001). The figure shows the HR plotted for each HLA locus using a linear spline with a knot at 5 AA mm.
Thus, The risk of GF adjusted for donor and recipient covariates, including HLA antigen mm, significantly increases with the number of AA mm at HLA-DR.
To cite this abstract in AMA style:
Kamoun M, McCullough K, Maiers M, Fernandez-Vina M, Li H, Leichtman A, Merion R. Association of HLA Amino Acid Mismatches with Kidney Allograft Failure [abstract]. Am J Transplant. 2013; 13 (suppl 5). https://atcmeetingabstracts.com/abstract/association-of-hla-amino-acid-mismatches-with-kidney-allograft-failure/. Accessed January 9, 2026.« Back to 2013 American Transplant Congress
