Living Kidney Donors Who Lose Weight in Order to Be Able to Donate, Gain More Weight after Donation
Department of Nephrology, Renal Transplant and Urology, Guy's and St. Thomas' NHS Foundation Trust, London, United Kingdom
Meeting: 2019 American Transplant Congress
Abstract number: 447
Keywords: Donation, Kidney transplantation, Obesity
Session Information
Session Name: Concurrent Session: Kidney Living Donor: Long Term Outcomes
Session Type: Concurrent Session
Date: Tuesday, June 4, 2019
Session Time: 2:30pm-4:00pm
 Presentation Time: 2:54pm-3:06pm
Presentation Time: 2:54pm-3:06pm
Location: Room 304
*Purpose: Living donor kidney transplantation is widely accepted to be the treatment of choice for end-stage kidney disease, and great efforts are undertaken to expand living donor kidney transplantation programmes. However, in recent years data have emerged that have led to an increased awareness of the potential long-term risks for kidney donors. Kidney donors are now widely counselled of the increased risk of end-stage kidney disease. In line with changes in the general population, an increased proportion of live donor candidates are now overweight or obese. Obesity has been shown to be an independent risk factor for the development of ESRD, as well as for the development of type 2 diabetes. Our living donor programme concentrates much effort on lifestyle modification in live donor candidates, focusing on weight loss, smoking cessation and the benefits of exercise. No data are currently available as to whether these recommendations are followed by live donors after donation.
*Methods: We conducted a retrospective analysis of all live donors who proceeded to donation in the years 2014-15, and who were followed up for at least 2 years in our centre. Comparisons in donors’ BMI over this period were made with matched pair analysis from initial assessment to preoperative assessment, 1 year and 2 years after donation.
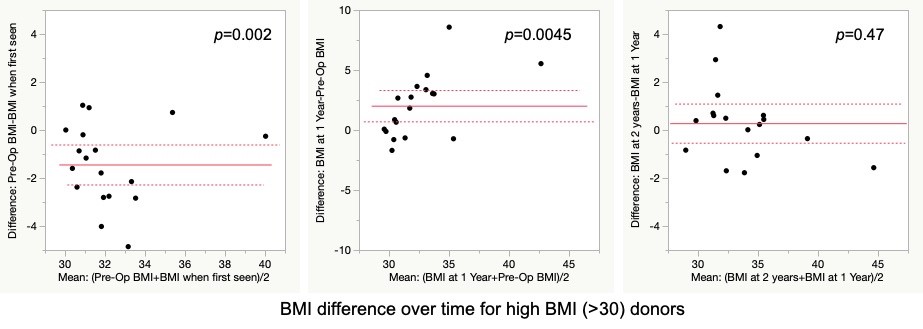
*Results: Our data demonstrate that at the time of first contact with the LD team, 63/132 donors (47.8%) had a body mass index (BMI) between 25-30 kg/m2, and 18/132 (13.6%) had a BMI of >30 mg/m2. Those donors with a BMI >30 kg/m2 at presentation were seen to lose weight by the time of surgery (mean change in BMI -1.5, p=0.002). However, data at 1 year follow-up shows that the donors with BMI >30 at presentation gained weight after donation (mean change in BMI +2.0 p=0.0045), returning to their initial weight. These patients maintain their weight at 2 years (mean BMI difference 0.29; p=0.47). No significant change in weight was seen in donors with BMI <30 at presentation. There were no new diagnoses of type 2 diabetes in this time.
*Conclusions: These data underline the difficulties in maintaining lifestyle modifications, even in highly motivated and selected individuals. The impact of weight gain on long-term donor risk needs further evaluation, and live donor programmes should consider continuing to provide support with lifestyle modification after donation.
To cite this abstract in AMA style:
Punjala SR, Silas L, Gokmen R, Karydis N. Living Kidney Donors Who Lose Weight in Order to Be Able to Donate, Gain More Weight after Donation [abstract]. Am J Transplant. 2019; 19 (suppl 3). https://atcmeetingabstracts.com/abstract/living-kidney-donors-who-lose-weight-in-order-to-be-able-to-donate-gain-more-weight-after-donation/. Accessed February 18, 2026.« Back to 2019 American Transplant Congress