The Evolving Clinical Presentation of Acute Rejection in Face Transplantation
Plastic and Reconstructive Surgery, Brigham and Women's Hospital, Boston, MA
Meeting: 2019 American Transplant Congress
Abstract number: 308
Keywords: Immunosuppression, Monitoring, Rejection
Session Information
Session Name: Concurrent Session: Basic & Clinical Science - VCA
Session Type: Concurrent Session
Date: Monday, June 3, 2019
Session Time: 2:30pm-4:00pm
 Presentation Time: 3:42pm-3:54pm
Presentation Time: 3:42pm-3:54pm
Location: Room 209
*Purpose: Clinical signs such as erythema or edema are traditionally helpful to diagnose Acute rejection (AR) in face transplantation (FT) in the early follow-up. The study’s purpose was to evaluate, whether these clinical signs remain reliable markers of acute rejection beyond the second post-transplant year.
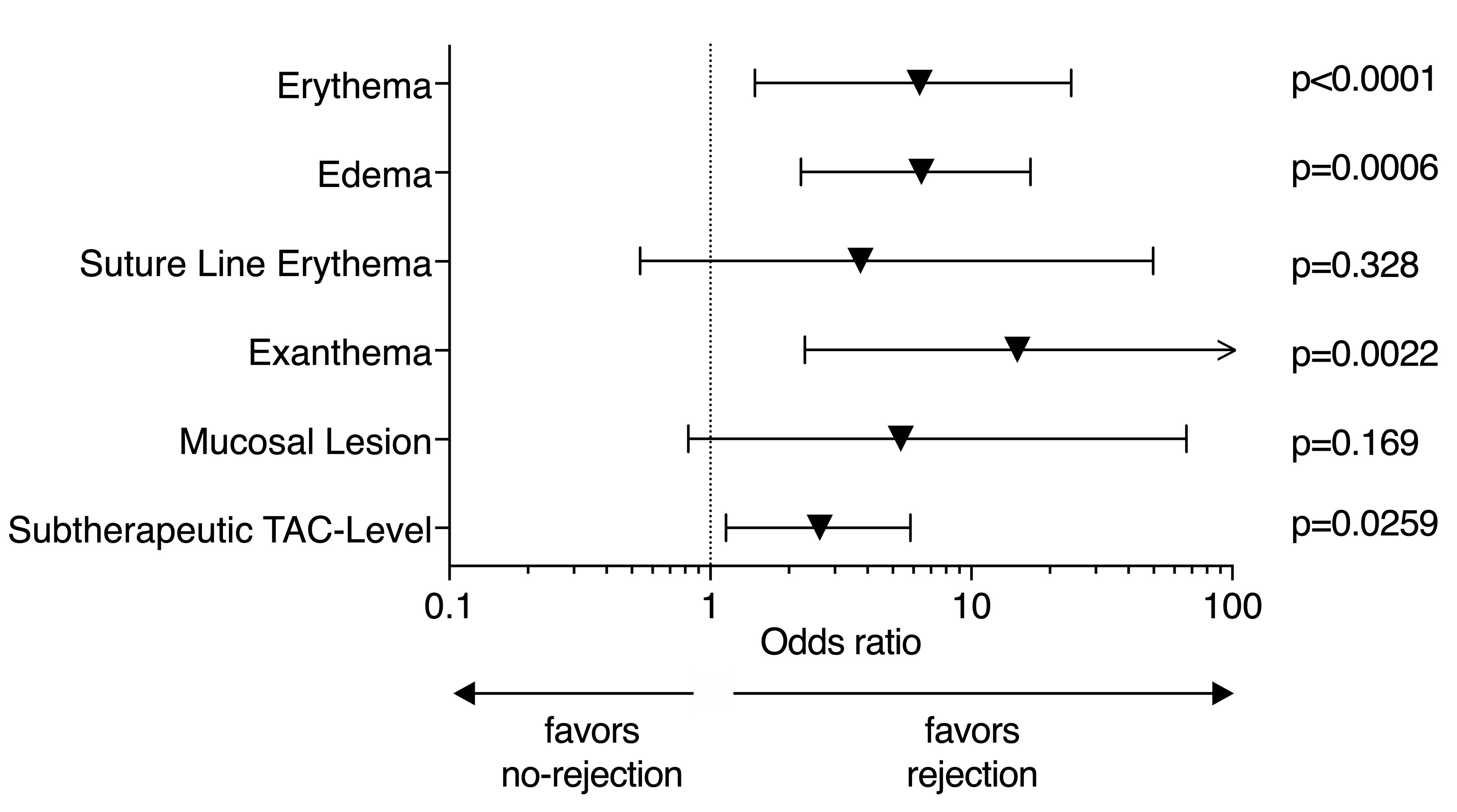
*Methods: We conducted a retrospective study of seven FT recipients, who underwent full or partial FT between April 2009 and October 2014, with up to 8-year follow-up to determine the diagnostic value of clinical signs of AR over time. Five clinical signs of AR were evaluated: erythema, edema, exanthema, suture line erythema and mucosal lesions. Odds ratios (OR) were calculated to determine the statistically significant association of these signs with histopathological diagnosis of rejection according to the Banff-Classification.
*Results: We identified 104 clinical encounters. Following indicators showed a significant correlation with episodes of AR (Fig.1): erythema (OR 6.33, 95% CI 1.48 – 24.15), edema (OR 6.43, 95% CI 2.23 – 16.87), exanthema (OR 15, 95% CI 2.3 – 166) and subtherapeutic tacrolimus levels (OR 2.63, 95% CI 1.15 -5.85). On the other hand, suture line erythema (OR 3.77, 95% CI 0.54 – 49.7) and mucosal lesions (OR 2.63, 95% CI 0.82 – 66.66) did not show a significant correlation with episodes of AR. Beyond two years post transplantation, only erythema (p=0.0042) and exanthema (p=0.0036) demonstrated to be reliable clinical signs of AR in FT. In addition, occurrence of subclinical rejection was more frequent during later follow-up time-points (24% of late rejections vs. 6% of early rejections). Subclinical rejection occurred at least once in every patient except patient 6. Taking all 46 rejection episodes into account, 8 presented subclinically (17.4%). Of them, 1 occurred in the early period (12.5%) and 7 occurred in the late period (87.5%). Subclinical rejection represented 24% of late rejection episodes but only 6% of early rejection episodes. Interestingly, 62.5% of subclinical rejections (5 out of 8) were associated with subtherapeutic tacrolimus levels.
*Conclusions: In summary, our findings suggest that AR in the FT context becomes less macroscopically ascertainable and accordingly more difficult to diagnose over time, particularly after the second postoperative year. Until alternative biomarkers for rejection are identified, protocol biopsies will remain critical for guiding assessments of allograft rejection.
To cite this abstract in AMA style:
Haug V, Kollar B, Obed D, Kiwanuka H, Turk M, Wo L, Tasigiorgos S, Kueckelhaus M, Riella L, Pomahac B. The Evolving Clinical Presentation of Acute Rejection in Face Transplantation [abstract]. Am J Transplant. 2019; 19 (suppl 3). https://atcmeetingabstracts.com/abstract/the-evolving-clinical-presentation-of-acute-rejection-in-face-transplantation/. Accessed January 28, 2026.« Back to 2019 American Transplant Congress