Circulating Donor Specific Antibody and Biopsy C4d Positivity in Pancreas Rejection Increase the Probability of Earlier Return to Insulin after Rejection
1Medicine, University of Minnesota, Minneapolis, MN, 2Complex Care Analytics, Fairview Health Services, Minneapolis, MN, 3Surgery, University of Minnesota, Minneapolis, MN
Meeting: 2019 American Transplant Congress
Abstract number: 196
Keywords: Alloantibodies, CD4, Pancreas transplantation, Rejection
Session Information
Session Name: Concurrent Session: Pancreas and Islet: All Topics I
Session Type: Concurrent Session
Date: Sunday, June 2, 2019
Session Time: 4:30pm-6:00pm
 Presentation Time: 4:54pm-5:06pm
Presentation Time: 4:54pm-5:06pm
Location: Room 209
*Purpose: Outcome data following rejection in pancreas recipients are sparse. We sought to study the influence of C4d positivity and the presence of circulating DSA on the probability of becoming insulin dependent after initial rejection and the probability of recurrent rejection after initial rejection.
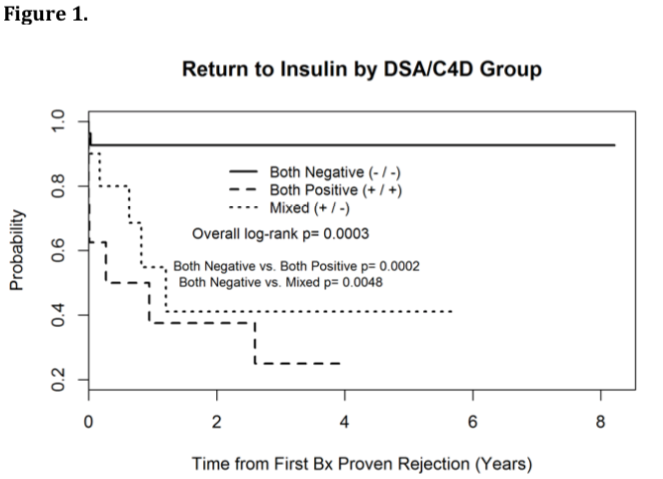
*Methods: A retrospective analysis of 272 primary simultaneous kidney and pancreas (SPK) and pancreas alone transplant (PAT) recipients from 1/1/2009 to 3/31/2018. Of these 53 recipients were treated for acute pancreas rejection. The presence of C4d staining on biopsy, circulating donor specific antibodies (DSA) and the date of return to insulin were identified. 8 subjects were excluded due to missing C4d staining. C4d status and circulating DSA grouped the subjects into 3 groups: C4d and DSA negative (-/-), C4d and DSA Positive (+/+), and either alone positive (+/-). Kaplan Meier curves were created to examine the probability of becoming insulin dependent after the initial rejection and the probability of recurrent rejection after initial rejection episode.
*Results: Out of 45 unique initial pancreas rejection episodes in SPK and PAT recipients, 27 recipients were in (-/-) group, 10 recipients were in (-/+) group, and 8 recipients were in (+/+) group. Estimates of insulin free survival at one-year post rejection were 93% (-/-), 55% (+/-), and 38% (+/+). There were significant differences in overall insulin free survival among groups (figure 1, log-rank p<0.001). Pairwise differences occurred for the both negative group vs. the positive and mixed groups (adjusted p<0.01). Estimates of recurrent rejection free survival at one-year post-rejection were 85% (-/-), 60% (+/-) and 63% (+/+). There was no difference in overall recurrent rejection free survival (figure 2, log-rank p=0.29).
*Conclusions: In the settings of initial acute rejection, the absence of both circulating DSA and C4d positivity, compared to the presence of circulating DSA and/or C4d positivity, is associated with a lower risk of return to insulin dependence (surrogate of pancreas graft loss), but not the risk of recurrent rejection in the year following the initial episode. More studies are needed to identify and validate predictors of the point of no return to help inform the decision to treat and perhaps the choice of treatment.
To cite this abstract in AMA style:
Riad SM, Jackson S, Finger EB, Kandaswamy R. Circulating Donor Specific Antibody and Biopsy C4d Positivity in Pancreas Rejection Increase the Probability of Earlier Return to Insulin after Rejection [abstract]. Am J Transplant. 2019; 19 (suppl 3). https://atcmeetingabstracts.com/abstract/circulating-donor-specific-antibody-and-biopsy-c4d-positivity-in-pancreas-rejection-increase-the-probability-of-earlier-return-to-insulin-after-rejection/. Accessed February 18, 2026.« Back to 2019 American Transplant Congress