Recipient ABO Blood-Type is Associated with Their Survival after Adult-to-Adult Living-Donor Liver Transplantation: Blood-Type O is Disadvantage?
T. Goto,1 K. Hata,1 M. Nagao,2 J. Kusakabe,1 Y. Okamura,1 T. Tajima,1 I. Tamaki,1 Y. Nigmet,1 T. Tajima,1 J. Yoshikawa,1 H. Tanaka,1 S. Ichiyama,2 S. Uemoto.1
1Division of Hepato-Biliary-Pancreatic Surgery and Transplantation, Department of Surgery, Graduate School of Medicine, Kyoto University, Kyoto City, Japan
2Department of Infection Control and Prevention, Kyoto University Hospital, Kyoto City, Japan.
Meeting: 2018 American Transplant Congress
Abstract number: D229
Keywords: Liver failure, Living-related liver donors, Mortality, Risk factors
Session Information
Session Name: Poster Session D: Liver: Living Donors and Partial Grafts
Session Type: Poster Session
Date: Tuesday, June 5, 2018
Session Time: 6:00pm-7:00pm
 Presentation Time: 6:00pm-7:00pm
Presentation Time: 6:00pm-7:00pm
Location: Hall 4EF
PURPOSE: Accumulating evidence has suggested that ABO blood-type is associated with the prevalence and severity of infectious diseases, cancers, and cardiovascular diseases, however, its impact on organ transplantation remains unclear.
METHODS: We retrospectively analyzed 557 consecutive cases of primary adult-to-adult living-donor liver transplantation (LDLT) from January 2000 to June 2014 in our center. ABO-incompatible cases were all excluded from this study to eliminate the influence from antibody-mediated rejection and the different immunosuppression regimens. Recipients were thus divided into 4 groups according to recipients' ABO blood-type: Group-A (n = 246); Group-B (n = 107); Group-O (n = 147); and Group-AB (n = 57). The primary end point was recipient survival. Secondly, we investigated patients' backgrounds and various clinical factors which could be extracted from electronic medical records after 2006, including 258 recipients.
RESULTS: In whole recipients' survival, there was significant difference among four groups (P = 0.028, Figure-1A), which was more prominent in comparison between Group-O and the others (P = 0.004, Figure-1B).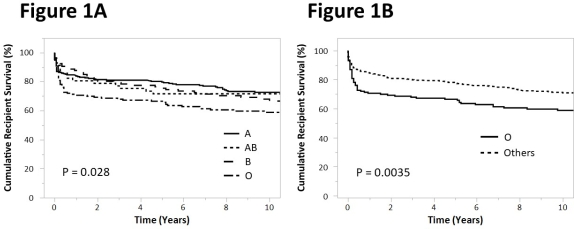 258 recipients' analysis revealed that there was no significant difference in patients' backgrounds between Group-O and the others, including recipients' age & sex, donor age, etiologies, and MELD scores. Recipient survival in Group-O was significantly worse than others (P = 0.035, hazard ratio 1.75; 95% Confidence Interval, 1.04-2.87, Figure-2).
258 recipients' analysis revealed that there was no significant difference in patients' backgrounds between Group-O and the others, including recipients' age & sex, donor age, etiologies, and MELD scores. Recipient survival in Group-O was significantly worse than others (P = 0.035, hazard ratio 1.75; 95% Confidence Interval, 1.04-2.87, Figure-2).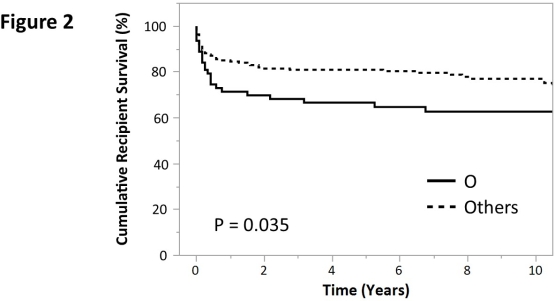 Univariate and multivariate analyses both demonstrated recipients' blood-type O (P = 0.005; OR: 3.91 95%CI: 1.49-10.26), donor age (P = 0.006; OR: 1.05; 95%CI: 1.01-1.10), not right-lobe graft (P < 0.001; OR:6.16; 95%CI: 2.39-15.82), operation time (P = 0.033; OR: 0.81; 95%CI: 0.66-0.99), post-transplant bacteremia (P < 0.001; OR: 1.52; 95%CI: 1.24-1.86), counts of pulsed steroid therapy (P < 0.001; OR: 3.12; 95%CI: 1.53-6.34), and counts of acute rejection (P < 0.001; OR: 0.24; 95%CI: 0.11-0.52),were identified as independent risk factors for 1-year survival.
Univariate and multivariate analyses both demonstrated recipients' blood-type O (P = 0.005; OR: 3.91 95%CI: 1.49-10.26), donor age (P = 0.006; OR: 1.05; 95%CI: 1.01-1.10), not right-lobe graft (P < 0.001; OR:6.16; 95%CI: 2.39-15.82), operation time (P = 0.033; OR: 0.81; 95%CI: 0.66-0.99), post-transplant bacteremia (P < 0.001; OR: 1.52; 95%CI: 1.24-1.86), counts of pulsed steroid therapy (P < 0.001; OR: 3.12; 95%CI: 1.53-6.34), and counts of acute rejection (P < 0.001; OR: 0.24; 95%CI: 0.11-0.52),were identified as independent risk factors for 1-year survival.
CONCLUSION: Recipient blood-type O was an independent risk factor in adult-to-adult LDLT.
CITATION INFORMATION: Goto T., Hata K., Nagao M., Kusakabe J., Okamura Y., Tajima T., Tamaki I., Nigmet Y., Tajima T., Yoshikawa J., Tanaka H., Ichiyama S., Uemoto S. Recipient ABO Blood-Type is Associated with Their Survival after Adult-to-Adult Living-Donor Liver Transplantation: Blood-Type O is Disadvantage? Am J Transplant. 2017;17 (suppl 3).
To cite this abstract in AMA style:
Goto T, Hata K, Nagao M, Kusakabe J, Okamura Y, Tajima T, Tamaki I, Nigmet Y, Tajima T, Yoshikawa J, Tanaka H, Ichiyama S, Uemoto S. Recipient ABO Blood-Type is Associated with Their Survival after Adult-to-Adult Living-Donor Liver Transplantation: Blood-Type O is Disadvantage? [abstract]. https://atcmeetingabstracts.com/abstract/recipient-abo-blood-type-is-associated-with-their-survival-after-adult-to-adult-living-donor-liver-transplantation-blood-type-o-is-disadvantage/. Accessed May 9, 2025.« Back to 2018 American Transplant Congress
