Significance of an Isolated Elevated PRA in Renal Transplantation
Houston Methodist Hospital, Houston, TX.
Meeting: 2015 American Transplant Congress
Abstract number: D154
Keywords: Panel reactive antibodies, Rejection
Session Information
Session Name: Poster Session D: Kidney: Acute Rejection
Session Type: Poster Session
Date: Tuesday, May 5, 2015
Session Time: 5:30pm-6:30pm
 Presentation Time: 5:30pm-6:30pm
Presentation Time: 5:30pm-6:30pm
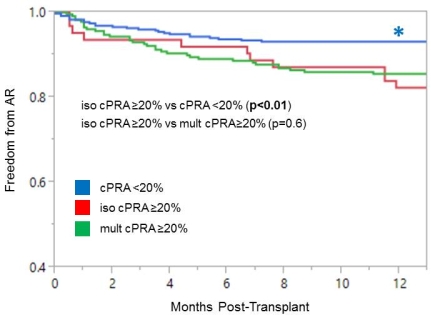
Location: Exhibit Hall E
Transplant centers have traditionally discerned a patient's immunologic risk based on peak panel reactive antibody (PRA) levels. However, in a given patient, pre-transplant PRA may fluctuate and it is unclear whether patients with a single elevated PRA impose the same immunologic risk as those with multiple elevated PRA. The purpose of this study was to compare graft outcomes among renal transplant recipients (RTRs) with an isolated calculated PRA ≥20% (iso cPRA ≥20), multiple cPRA ≥20% (mult cPRA ≥20), or all cPRA <20% (cPRA <20). RTRs from 6/2008 to 9/2013 were reviewed; only patients with at least 2 or more pre-transplant cPRA measurements were included. Baseline demographics are shown below. Compared to patients with cPRA <20, those with iso cPRA ≥20 were more likely to be African American and deceased donor recipients. In contrast, there were significantly fewer female recipients and re-transplants in the iso cPRA ≥20 group compared to mult PRA ≥20 patients. At 1 year, iso cPRA ≥20 experienced significantly higher acute rejection (AR) (19%) than cPRA <20 (7%, p<0.01) but similar rates to mult cPRA ≥20 (14%, p=0.4). Rates of de novo donor specific antibody and antibody-mediated rejection at 1 year did not differ among groups (17%, 20%, 26% [p=NS] and 0.6%, 1.6%, 6% [p=NS]). Conversely, one-year graft survival was higher in iso cPRA ≥20 compared to the mult cPRA ≥20 group (98% vs. 88%, p=0.02). In conclusion, although patients with iso cPRA ≥20 are demographically different than those with mult cPRA ≥20, AR at 1 year was comparable. Our data suggests that even a single elevated PRA carries a similar immunologic risk as multiple elevated PRAs in renal transplantation.
| cPRA <20 (n=359) [A] | iso cPRA ≥20 (n=64) [B] | mult cPRA ≥20 (n=238) [C] | p-value [A vs B] | p-value [B vs C] | |
| Total # Pre-Transplant cPRA | 4.3 | 5.0 | 6.5 | 0.08 | <0.01 |
| Age (years) | 51.2 | 48.8 | 49.4 | 0.18 | 0.71 |
| Female (%) | 33 | 38 | 60 | 0.5 | <0.01 |
| AA (%) | 19 | 37 | 35 | <0.01 | 0.81 |
| Peak cPRA I (%) | 13.1 | 21.5 | 34.6 | <0.01 | <0.01 |
| Peak cPRA II (%) | 13.0 | 27.5 | 40.6 | <0.01 | <0.01 |
| Re-transplant (%) | 2 | 3 | 15 | 0.66 | <0.01 |
| Deceased donor (%) | 50 | 64 | 77 | 0.03 | 0.03 |
To cite this abstract in AMA style:
Kuten S, Patel S, Land G, Eagar T, Knight R, Loucks J, Gaber L, Gaber A. Significance of an Isolated Elevated PRA in Renal Transplantation [abstract]. Am J Transplant. 2015; 15 (suppl 3). https://atcmeetingabstracts.com/abstract/significance-of-an-isolated-elevated-pra-in-renal-transplantation/. Accessed February 4, 2026.« Back to 2015 American Transplant Congress
