The Fate of Older Candidates Referred for Kidney Transplantation
Vanderbilt University Medical Center, Nashville, TN.
Meeting: 2018 American Transplant Congress
Abstract number: A319
Keywords: Elderly patients, Outcome, Waiting lists
Session Information
Session Name: Poster Session A: Non-Organ Specific: Disparities to Outcome and Access to Healthcare
Session Type: Poster Session
Date: Saturday, June 2, 2018
Session Time: 5:30pm-7:30pm
 Presentation Time: 5:30pm-7:30pm
Presentation Time: 5:30pm-7:30pm
Location: Hall 4EF
Background: Older ESRD/CKD patients have reduced access to transplantation compared to younger counterparts as measured by waitlisting and transplantation rates. This is true even in those with excellent predicted posttransplant survival. Among those referred to a transplant center, the fate of older kidney transplant candidates has not been well described.
Methods: We retrospectively reviewed patients >65 yrs evaluated at an academic center in 2011-14 for kidney transplantation. Patient characteristics were collected via chart review. Based on published literature, predicted 3-yr posttransplant survival for each patient was calculated and patients were risk categorized as having excellent, good or not excellent/good predicted survival. Transplant evaluation outcomes were determined via chart review. A multivariate logistic regression analysis was used to quantify the association of baseline patient characteristics and the outcomes of waitlisting and transplantation.
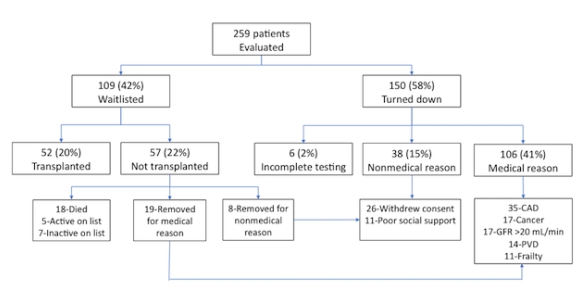
Results: The cohort consisted of 259 older patients with the following characteristics: mean age 69 yrs, 57% male, mean dialysis vintage 21 mos, 51% DM, 34% CAD, 31% excellent predicted survival, mean predicted 3-yr survival 81%. Transplant evaluation outcomes are shown in figure.
The most common medical and non-medical reasons for being turned down or removed from the waitlist were CAD and withdrawal of consent, respectively. Multivariate logistic regression showed that older age (p<0.001), longer dialysis vintage (p=0.002), CAD (p=0.03) and smoking history (p=0.04) were associated with reduced odds of being waitlisted. Only age was significantly associated with transplantation (OR 0.83 [95% CI 0.78-0.93], p=0.012). Predicted 3-yr posttransplant survival and risk category were associated with waitlisting (both p<0.001) but not transplantation (p=0.166 and p=0.189, respectively).
Conclusion: In this cohort, age at time of referral was the most important predictor for waitlisting and transplantation. Important reasons for patients being turned down or removed from the waitlist were CAD and withdrawal of consent. This study provides some insight on pretransplant factors that influence older candidates' access to kidney transplantation.
CITATION INFORMATION: Shwetar M., Abdel-Kader K., Concepcion B. The Fate of Older Candidates Referred for Kidney Transplantation Am J Transplant. 2017;17 (suppl 3).
To cite this abstract in AMA style:
Shwetar M, Abdel-Kader K, Concepcion B. The Fate of Older Candidates Referred for Kidney Transplantation [abstract]. https://atcmeetingabstracts.com/abstract/the-fate-of-older-candidates-referred-for-kidney-transplantation/. Accessed January 5, 2026.« Back to 2018 American Transplant Congress