Living Kidney Donation: Impact of Transplant Center Labor, Organization, and Resources
1Vanderbilt University, Nashville
2Montana State University, Bozeman
3Beth Israel Deaconess, Boston.
Meeting: 2018 American Transplant Congress
Abstract number: 533
Keywords: Donation, Kidney, Resource utilization
Session Information
Session Name: Concurrent Session: Kidney Living Donation: Programmatic Issues
Session Type: Concurrent Session
Date: Tuesday, June 5, 2018
Session Time: 4:30pm-6:00pm
 Presentation Time: 5:18pm-5:30pm
Presentation Time: 5:18pm-5:30pm
Location: Room 6B
Purpose: Impact of transplant center program size, staffing, and organization on LKD outcomes is unknown. This study describes the labor inputs, organization, and resources available within U.S. living donor (LD) programs and their associations with LD outcomes.
Method: A survey was sent to the living donor coordinator (LDC) at every U.S. LD program (n=211; RR=70%, total respondents=148). Respondent surveys were linked to AHA and SRTR databases to describe hospital characteristics and volumes. Descriptive statistics summarized responses; multiple linear regressions assessed associations of center characteristics with outcome variables.
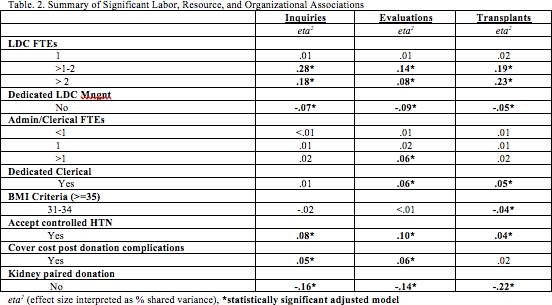
Results: 74% of programs reported dedicated LDCs (Table 1). Median LDC FTEs per center was 1.0 (IQR 1-2); 37% of programs reported that the LDC devoted < 40 hours per week to the LD program. >1 LDC FTE was associated with higher numbers of LD inquires, evaluations, and transplants, as was having a dedicated LDC (p<0.004) (Table 2). Dedicated LD clerical staff was associated with higher numbers of evaluations and transplants (p<0.003). Centers that accept donors with controlled HTN and centers that have a KPD program reported higher LD inquires, evaluations, and transplants (p<0.021). The overall national conversion rate from initial contact to LD transplant was 8% and from evaluation to LD transplant was 32%.
Conclusion: Findings suggest an association of labor, organizational and resource inputs with LD outcomes suggesting that centers invest in nursing and non-nursing staffing, evaluate donor management structure, review acceptance criteria/protocols, and devote specific resources to the LD program. This is the first known study in the transplant literature that describes an association between nurse labor and LD outcomes.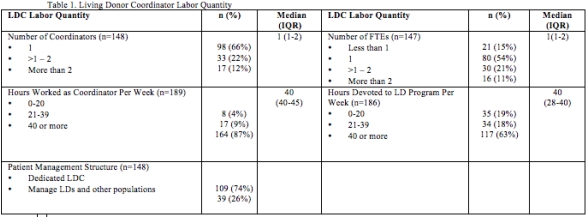
CITATION INFORMATION: Moore D., Dietrich M., Buerhaus P., Rodrigue J., Minnick A. Living Kidney Donation: Impact of Transplant Center Labor, Organization, and Resources Am J Transplant. 2017;17 (suppl 3).
To cite this abstract in AMA style:
Moore D, Dietrich M, Buerhaus P, Rodrigue J, Minnick A. Living Kidney Donation: Impact of Transplant Center Labor, Organization, and Resources [abstract]. https://atcmeetingabstracts.com/abstract/living-kidney-donation-impact-of-transplant-center-labor-organization-and-resources/. Accessed February 17, 2026.« Back to 2018 American Transplant Congress
