Association of Health Literacy with Adverse Outcomes among Kidney Transplant Candidates and Recipients
F. Warsame, C. Haugen, J. Garonzik-Wang, N. Desai, D. Crews, T. Purnell, M. McAdams-DeMarco, D. Segev.
Johns Hopkins University, Baltimore, MD.
Meeting: 2018 American Transplant Congress
Abstract number: 225
Keywords: Kidney transplantation, Outcome, Risk factors
Session Information
Session Name: Concurrent Session: Kidney Psychosocial - 2
Session Type: Concurrent Session
Date: Monday, June 4, 2018
Session Time: 2:30pm-4:00pm
 Presentation Time: 2:30pm-2:42pm
Presentation Time: 2:30pm-2:42pm
Location: Room 210
Limited health literacy (LHL) is known to adversely affect health outcomes in patients managing chronic illness. We aimed to examine the association between LHL, listing, and waitlist mortality among KT candidates, as well between LHL and postoperative length of stay among KT recipients.
Methods: In a prospective cohort study of 1,544 KT adult candidates and 379 KT recipients, health literacy was assessed at the time of KT evaluation and at admission for KT, respectively (5/2014-8/2017). LHL was identified using the Brief Health Literacy Screen (BHLS; scores range from 0-12, with higher scores indicating worse health literacy). Based on the distribution of scores in each cohort, a BHLS score>7 in KT Candidates and a BHLS score>5 in KT Recipients were used to define LHL. Using Cox proportional hazards models, adjusted for demographic and clinical characteristics, we quantified the association between LHL with time to listing and waitlist mortality among KT candidates and between LHL and length of KT hospital stay among KT recipients.
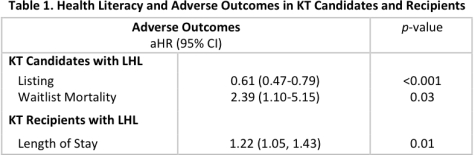
Results: 9.3% of all KT candidates and 7.2% of KT patients on the KT waitlist had LHL (BHLS>7). Among KT candidates, a 1-point increase in BHLS score was associated with a 5.5% decreased risk of listing (aHR=0.945, 95%CI: 0.92-0.93, p<0.001). Candidates with LHL had a 39% decreased risk of listing and a 2.39-fold increased risk of waitlist mortality (Table 1). 15.6% of KT recipients had LHL (BHLS>5). In KT recipients, a 1-point increase in BLHS was associated with 1.02-fold (95%CI: 1.01-1.05, p=0.04) longer length of stay, and KT recipients with LHL had a 1.22-fold (95%CI: 1.05-1.43, p=0.01) longer length of stay (Table 1).
Conclusion: KT Candidates with LHL are less likely to be listed for KT and those who are listed are at increased waitlist mortality risk. Those with LHL at the time of KT experience longer lengths of hospital stay. Overall, patients with LHL may represent a more vulnerable subgroup of KT candidates and recipients that require additional support and resources during transplant evaluation and discharge.
CITATION INFORMATION: Warsame F., Haugen C., Garonzik-Wang J., Desai N., Crews D., Purnell T., McAdams-DeMarco M., Segev D. Association of Health Literacy with Adverse Outcomes among Kidney Transplant Candidates and Recipients Am J Transplant. 2017;17 (suppl 3).
To cite this abstract in AMA style:
Warsame F, Haugen C, Garonzik-Wang J, Desai N, Crews D, Purnell T, McAdams-DeMarco M, Segev D. Association of Health Literacy with Adverse Outcomes among Kidney Transplant Candidates and Recipients [abstract]. https://atcmeetingabstracts.com/abstract/association-of-health-literacy-with-adverse-outcomes-among-kidney-transplant-candidates-and-recipients/. Accessed January 29, 2026.« Back to 2018 American Transplant Congress