A Propensity Matched Survival Analysis: Do Simultaneous Liver-Lung Transplant Recipients Need a Liver?
1School of Medicine, Duke University, Durham, NC
2Surgery, Duke University, Durham, NC.
Meeting: 2018 American Transplant Congress
Abstract number: 80
Keywords: Multivisceral transplantation, Outcome, Survival
Session Information
Session Name: Concurrent Session: Lung: From Allocation to Outcomes
Session Type: Concurrent Session
Date: Sunday, June 3, 2018
Session Time: 2:30pm-4:00pm
 Presentation Time: 3:30pm-3:42pm
Presentation Time: 3:30pm-3:42pm
Location: Room 303
Objective: There is debate whether simultaneous lung-liver transplant (LLT) long-term outcomes warrant allocation of two organs to a single recipient. We hypothesized that LLT recipients would have improved survival compared to matched single-organ lung recipients with a similar degree of liver dysfunction and tested this question using a large national database.
Methods: The OPTN/UNOS STAR file was queried for adult recipients of LLT and isolated lung transplant from 2006-2016. Unadjusted demographic characteristics were generated and examined. LLT recipients were matched 1:2 with single-organ lung recipients on age, gender, ethnicity, number of previous transplants, diagnosis, diabetes diagnosis, BMI, donor BMI, calculated MELDXI, lung allocation score (LAS), and year of transplant. Kaplan-Meier with log-rank compared survival between groups. Hazard ratios for transplant type were generated adjusting for age, gender, MELDXI, and LAS.
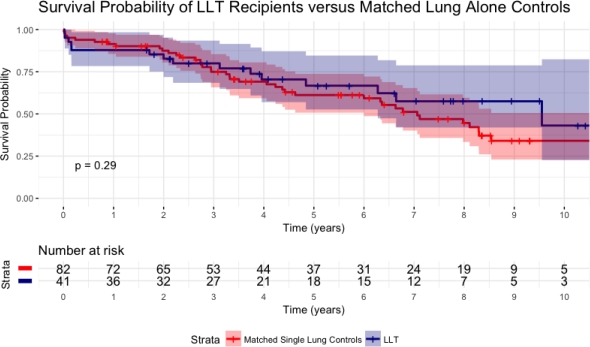
Results: Forty-one LLT patients were matched to eighty-two single-organ lung recipients on demographic characteristics, etiology, and liver and lung function at transplant. No differences in baseline characteristics or liver function were seen between the matched cohorts. Length of stay was significantly higher in LLT recipients compared to isolated lung recipients (44.60 days vs. 24.04 days, p=0.001). Functional follow-up status, acute rejection rate, and graft status at endpoint were not significantly different (all p>0.05). Overall survival was similar between matched lung alone and LLT (Figure 1, p=0.29). Adjusted hazard ratios did not show a change in survival risk for LLT versus single-organ transplant.
Conclusions: Survival in simultaneous LLT was comparable to isolated lung transplantation, even after matching for patient characteristics and level of liver dysfunction. LLT recipients, however, had a significantly longer length of stay representing more difficult post-operative course. Thus, this analysis failed to identify a cohort of patients that benefit significantly from LLT.
Figure 1: Ten-year Unadjusted Kaplan-Meier Overall Survival
CITATION INFORMATION: Freischlag K., Ezekian B., Schroder P., Mulvihill M., Knechtle S. A Propensity Matched Survival Analysis: Do Simultaneous Liver-Lung Transplant Recipients Need a Liver? Am J Transplant. 2017;17 (suppl 3).
To cite this abstract in AMA style:
Freischlag K, Ezekian B, Schroder P, Mulvihill M, Knechtle S. A Propensity Matched Survival Analysis: Do Simultaneous Liver-Lung Transplant Recipients Need a Liver? [abstract]. https://atcmeetingabstracts.com/abstract/a-propensity-matched-survival-analysis-do-simultaneous-liver-lung-transplant-recipients-need-a-liver/. Accessed February 16, 2026.« Back to 2018 American Transplant Congress