Polypharmacy and Frailty in Kidney Transplant Recipients.
Department of Surgery, Johns Hopkins Medicine Institute, Baltimore, MD
Meeting: 2017 American Transplant Congress
Abstract number: C133
Keywords: Kidney, Kidney transplantation, Risk factors
Session Information
Session Name: Poster Session C: Kidney Complications III
Session Type: Poster Session
Date: Monday, May 1, 2017
Session Time: 6:00pm-7:00pm
 Presentation Time: 6:00pm-7:00pm
Presentation Time: 6:00pm-7:00pm
Location: Hall D1
Frailty is common in kidney transplant (KT) recipients with a prevalence of 20%, and is associated with post-KT adverse events including mortality, DGF, early hospital readmissions and longer length of stay. Polypharmacy is frequent among frail older adults without ESRD. However, the association between number of medications and frailty among KT recipients is unclear.
738 participants were enrolled in a prospective cohort at the time of KT (12/2008-6/2016) and frailty status was measured immediately prior to KT. The number of prescription medications in the year before KT was analyzed as a count; polypharmacy was defined as 5-9 prescription medications, and hyperpolypharmacy as ≥ 10 prescription medications. Logistic regression was used to estimate the association between polypharmacy and frailty after adjusting for age, race, gender, BMI, donor type, time on dialysis and primary diagnosis.
The median number of medications in the year prior to KT was 5 (IQR, 0-10). 19.1% of the KT recipients had polypharmacy, while 28.2% of them had hyperpolypharmacy. Each additional prescribed medication was associated with 1.04-fold (95% CI, 1.01-1.07; p=0.013) increased odds of frailty at KT. Polypharmacy was associated with a 1.70-fold (95% CI, 1.01-2.88; p=0.047) higher odds of frailty at KT, and hyperpolypharmacy associated with a 2.30-fold (95% CI, 1.45-3.66; p=<0.001) higher odds. 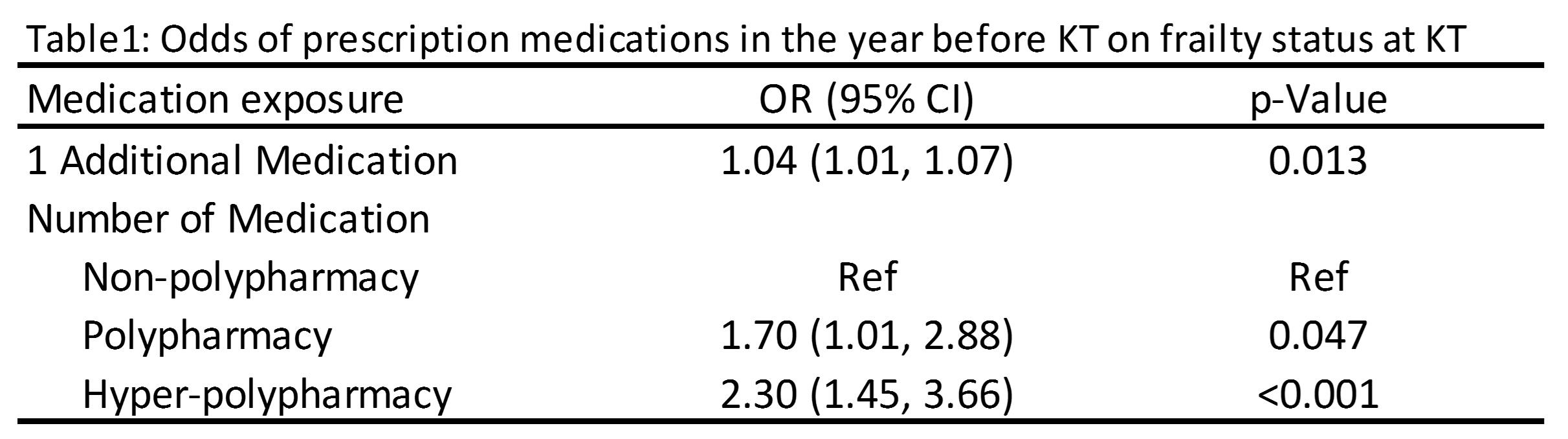 Anti-coagulants, pain control medications, or psychiatric/mental health medications were associated with a greater odds of frailty at KT.
Anti-coagulants, pain control medications, or psychiatric/mental health medications were associated with a greater odds of frailty at KT.  Frailty was more common among KT recipients with polypharmacy in the 1 year prior to KT. Individual classes of medications such as anti-coagulants, pain control medications, or psychiatric/mental health medications were also associated with a higher odds of frailty. Reducing medication use may help in halting or even reversing the development of frailty in KT recipients.
Frailty was more common among KT recipients with polypharmacy in the 1 year prior to KT. Individual classes of medications such as anti-coagulants, pain control medications, or psychiatric/mental health medications were also associated with a higher odds of frailty. Reducing medication use may help in halting or even reversing the development of frailty in KT recipients.
CITATION INFORMATION: Ying H, McAdams-DeMarco M, Segev D. Polypharmacy and Frailty in Kidney Transplant Recipients. Am J Transplant. 2017;17 (suppl 3).
To cite this abstract in AMA style:
Ying H, McAdams-DeMarco M, Segev D. Polypharmacy and Frailty in Kidney Transplant Recipients. [abstract]. Am J Transplant. 2017; 17 (suppl 3). https://atcmeetingabstracts.com/abstract/polypharmacy-and-frailty-in-kidney-transplant-recipients/. Accessed January 28, 2026.« Back to 2017 American Transplant Congress
