Photopheresis for Recalcitrant Rejection After Heart Transplantation: Worthwhile?
Cedars-Sinai Heart Institute, Los Angeles
Meeting: 2017 American Transplant Congress
Abstract number: C88
Keywords: Heart transplant patients, Immunosuppression
Session Information
Session Name: Poster Session C: Hearts and VADS: All Topics
Session Type: Poster Session
Date: Monday, May 1, 2017
Session Time: 6:00pm-7:00pm
 Presentation Time: 6:00pm-7:00pm
Presentation Time: 6:00pm-7:00pm
Location: Hall D1
Background: Rejection is leading cause of mortality after heart transplantation (HTx). While the rates of rejection have declined over the past few decades from improvement in immunosuppression, recalcitrant rejection still poses as a major problem for HTx recipients with high mortality. Photopheresis (Pph) is an immunomodatory therapy which involves treatment of leukocytes with psoralen and ultraviolet light. This therapy has been shown to be effective in patients with acute cellular rejection (ACR), antibody-mediated rejection (AMR), and biopsy negative rejection (BNR). We sought to establish the effectiveness of this immunosuppressive modality in our single center.
Methods: Between 2010-15 we assessed 458 HTx patients(pts) and found 17 pts who were treated with Pph for severe/recurrent rejection. Pph was administered for 2 consecutive days, weekly x4, and monthly x5. Pts were assessed for cardiac dysfunction and PRA pre- and post-therapy. Also assessed was subsequent 1-yr survival, 1-yr freedom from rejection (ACR, AMR, BNR), cardiac allograft vasculopathy as defined by stenosis ≥ 30% by angiography.
Results: For 17 pts treated with Pph, average time from Htx was 14 ± 10 mths. 35% pts had elevated Class I PRA prior to HTx, with a change from 43± 40% pre-Pph to 21 ± 37% post-Pph (p=0.339). 53% pts who had elevated Class II PRA prior to HTx had a trend from 66 ± 27% pre-Pph lowered to 22 ± 37% post-Pph (p=0.058). (Figure). There was no significant difference before and after therapy in LVEF (43 ± 14% vs 44 ± 16%, p=0.742). No pts developed ACR at subsequent 1-yr post-Pph and 1-yr freedom from AMR (94%) and BNR (79%) were less than pre-Pph. Subsequent 1-yr post-treatment survival, freedom from CAV were not unexpected (Table).
Conclusion: Pph for severe/recurrent rejection is associated with reasonable survival and appears effective at suppressing cellular/humoral responses. Further studies are warranted with a larger population size and longer follow-up to confirm these results.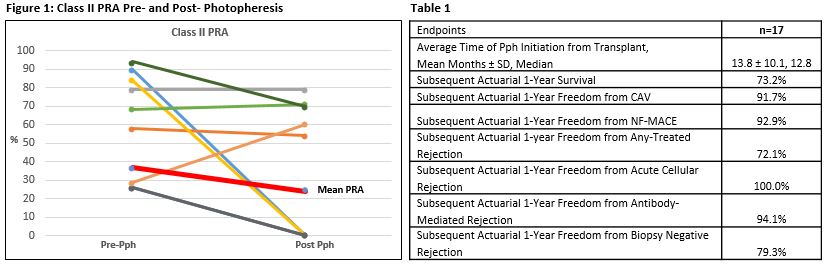
CITATION INFORMATION: Patel J, Kittleson M, Zhang X, Klapper E, Aintablian T, Murayama K, Czer L, Geft D, Chang D, Kobashigawa J. Photopheresis for Recalcitrant Rejection After Heart Transplantation: Worthwhile? Am J Transplant. 2017;17 (suppl 3).
To cite this abstract in AMA style:
Patel J, Kittleson M, Zhang X, Klapper E, Aintablian T, Murayama K, Czer L, Geft D, Chang D, Kobashigawa J. Photopheresis for Recalcitrant Rejection After Heart Transplantation: Worthwhile? [abstract]. Am J Transplant. 2017; 17 (suppl 3). https://atcmeetingabstracts.com/abstract/photopheresis-for-recalcitrant-rejection-after-heart-transplantation-worthwhile/. Accessed January 21, 2026.« Back to 2017 American Transplant Congress
