Disparities in Access to the Liver Transplant Wait List: A Statewide Analysis.
Surgery, Massachusetts General Hospital/Harvard Medical School, Boston, MA
Meeting: 2017 American Transplant Congress
Abstract number: C56
Keywords: Liver cirrhosis, Public policy, Risk factors, Waiting lists
Session Information
Session Name: Poster Session C: Disparity in Access and Outcomes for Solid Organ Transplantation
Session Type: Poster Session
Date: Monday, May 1, 2017
Session Time: 6:00pm-7:00pm
 Presentation Time: 6:00pm-7:00pm
Presentation Time: 6:00pm-7:00pm
Location: Hall D1
Background:Racial disparities in access to the liver transplant wait list for patients with end-stage liver disease (ESLD) are thought to be attributable to differences in demographics, primary diagnosis, and insurance patterns. We hypothesized that racial disparities would diminish by adjusting for gender, disease, and insurance.
Methods:ESLD patients were defined as age >18 with validated ICD-9 codes for cirrhosis as a primary diagnosis in the California Office of Statewide Health Planning and Development (OSHPD) inpatient database from 2000-2014. Patients on the liver transplant wait list were obtained from the UNOS Standard Transplant Analysis and Research for California (UNOS STAR CA). Patients previously transplanted or listed for a Status 1 liver were excluded. A wait list ratio (WLR) was calculated by obtaining the proportion of patients in UNOS STAR to those in OSHPD.
Results:There were 83461 patients with ESLD in California; however, only 13200 were waitlisted in UNOS STAR CA for an overall WLR of 0.16. WLRs were significantly different across race, with Asians having the highest WLR (0.30) compared to Whites (0.16), Blacks (0.11), and Hispanics (0.15) (all p<0.001). Gender, disease and insurance patterns were significantly different between race (all p<0.001). 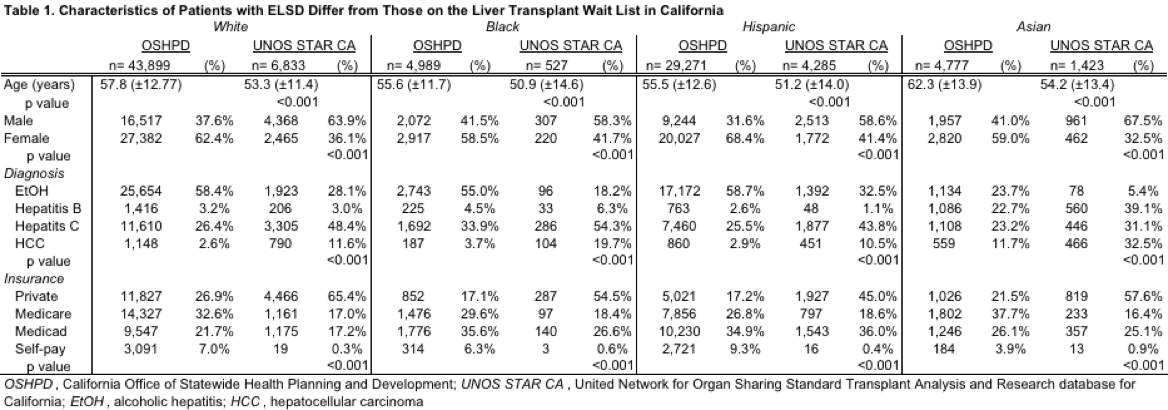 WLRs were significantly different even after stratifying by gender, diagnosis, and insurance (all p<0.001).
WLRs were significantly different even after stratifying by gender, diagnosis, and insurance (all p<0.001). 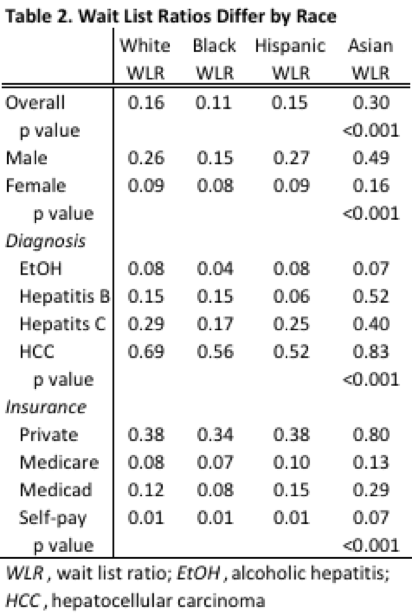 Conclusion:Fewer than 1 in 5 patients with ESLD make it to the wait list. Racial disparities in access to the liver transplant wait list persist across gender, diagnoses, and insurance patterns. As an ESLD registry does not exist, a quality improvement approach should consider benchmarking data to reduce variation in access to the liver transplant wait list across patient clinical and demographic characteristics.
Conclusion:Fewer than 1 in 5 patients with ESLD make it to the wait list. Racial disparities in access to the liver transplant wait list persist across gender, diagnoses, and insurance patterns. As an ESLD registry does not exist, a quality improvement approach should consider benchmarking data to reduce variation in access to the liver transplant wait list across patient clinical and demographic characteristics.
CITATION INFORMATION: Bababekov Y, Chang D, Hung Y.-C, Adler J, Stapleton S, Markmann J, Yeh H. Disparities in Access to the Liver Transplant Wait List: A Statewide Analysis. Am J Transplant. 2017;17 (suppl 3).
To cite this abstract in AMA style:
Bababekov Y, Chang D, Hung Y-C, Adler J, Stapleton S, Markmann J, Yeh H. Disparities in Access to the Liver Transplant Wait List: A Statewide Analysis. [abstract]. Am J Transplant. 2017; 17 (suppl 3). https://atcmeetingabstracts.com/abstract/disparities-in-access-to-the-liver-transplant-wait-list-a-statewide-analysis/. Accessed February 6, 2026.« Back to 2017 American Transplant Congress
