Use of Hepatitis C Infected Organs for Kidney Transplantation: A Medical Decision Analysis.
1Dalhousie University, Halifax, NS, Canada
2University of Alberta, Edmonton, AB, Canada
Meeting: 2017 American Transplant Congress
Abstract number: 493
Keywords: Allocation, Hepatitis C, Kidney transplantation, Outcome
Session Information
Session Name: Concurrent Session: DCD and Infectious Risk Kidney Donors
Session Type: Concurrent Session
Date: Tuesday, May 2, 2017
Session Time: 4:30pm-6:00pm
 Presentation Time: 5:30pm-5:42pm
Presentation Time: 5:30pm-5:42pm
Location: E450b
Given that Hepatitis C (HCV) can be cured, organs from HCV+ deceased donors might be used in HCV- recipients if treatment at the time of transplant is available and effective. The purpose of this analysis is to determine whether accepting a HCV+ organ is superior to waiting for a HCV- organ from the perspective of the recipient.
US mortality rates for wait-listed, functioning transplant and dialysis cohorts and graft survival rates were used for patient ages 20 to 75. Time 0 was the date of listing and patients were assumed to be on dialysis. The time horizon was 50 years and assumed no retransplantation. HCV– and HCV+ organs were assumed to be of similar quality. In the model, patients age 40 left on dialysis, with a HCV-kidney transplant or with HCV+ kidney transplant (untreated) were predicted to live 7.580, 13.266 or 11.773 years, respectively.
In this decision model, Option 1 patients on the waitlist would only opt to be transplanted with a HCV- organ (20% annual transplant rate = 5 years average wait). They were predicted to live 12.604 years (undiscounted). Option 2 patients opted to receive either a HCV- or HCV+ organ (annual transplant rate of 20% for a HCV- and 5% for a HCV+=average wait 4 years). Option 2 patients were transplanted on average a year earlier and lived 12.667 years (0.063 years more than Option1) assuming those who happened to get an HCV+ organ were cured with treatment. However for a 5% risk of treatment failure resulting in persistent HCV infection with an increased rate of death and graft loss then patients lived 12.655 years (0.051 years more than waiting for only a HCV- organ).
Conditions that would result in inferior outcomes were a short wait time advantage (<30 days) along with an HCV treatment failure rate of >10%; very high treatment failure rates with higher relative risks of death with persistent HCV infection (see figure); and patients<25 years of age with shorter wait times for a HCV- organ. 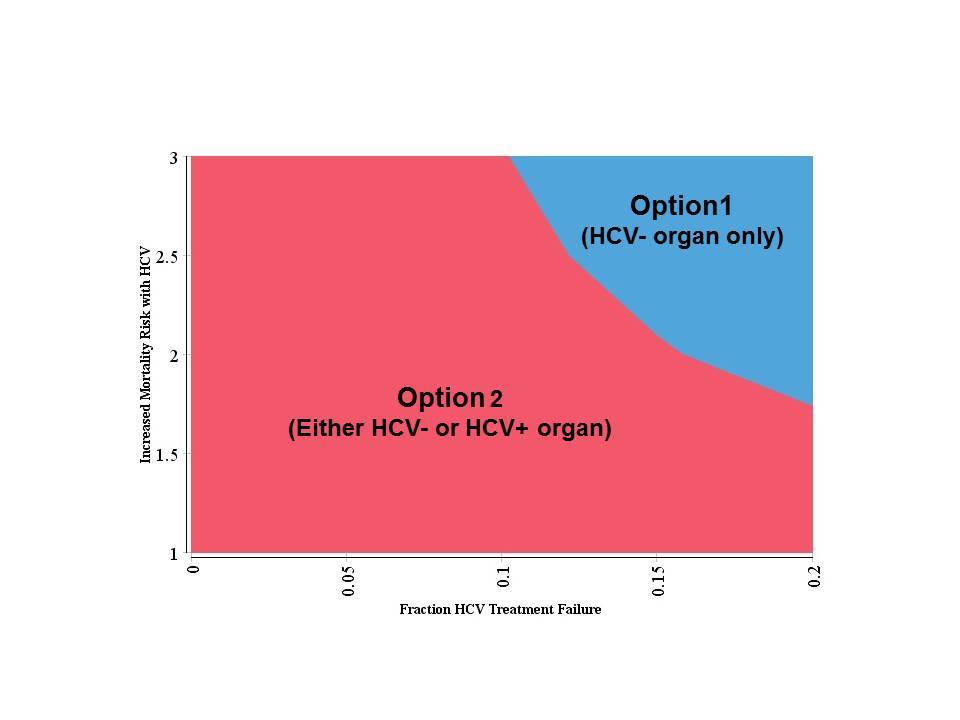 Under most assumptions the option of accepting a HCV+ organ with effective therapy with the hope of earlier transplantation will increase life years (patient perspective) and organ supply (societal perspective).
Under most assumptions the option of accepting a HCV+ organ with effective therapy with the hope of earlier transplantation will increase life years (patient perspective) and organ supply (societal perspective).
CITATION INFORMATION: Kiberd B, Doucette K, Tennankore K. Use of Hepatitis C Infected Organs for Kidney Transplantation: A Medical Decision Analysis. Am J Transplant. 2017;17 (suppl 3).
To cite this abstract in AMA style:
Kiberd B, Doucette K, Tennankore K. Use of Hepatitis C Infected Organs for Kidney Transplantation: A Medical Decision Analysis. [abstract]. Am J Transplant. 2017; 17 (suppl 3). https://atcmeetingabstracts.com/abstract/use-of-hepatitis-c-infected-organs-for-kidney-transplantation-a-medical-decision-analysis/. Accessed February 22, 2026.« Back to 2017 American Transplant Congress
