KDPI and Small (<20 kg) Pediatric Kidney Donors.
1Seattle Children's Hospital, Seattle
2Scientific Registry of Transplant Recipients, Minneapolis
Meeting: 2017 American Transplant Congress
Abstract number: 364
Keywords: Allocation, Donors, Kidney transplantation, marginal, Pediatric
Session Information
Session Name: Concurrent Session: Kidney: Pediatric Adherence and Allocation
Session Type: Concurrent Session
Date: Monday, May 1, 2017
Session Time: 4:30pm-6:00pm
 Presentation Time: 5:30pm-5:42pm
Presentation Time: 5:30pm-5:42pm
Location: E353B
Use of small (≤20 kg) donor kidneys in pediatric candidates has declined under the new kidney allocation system (KAS), from 5.0% of pediatric kidney-alone transplants pre-KAS to 1.7% post-KAS. One potential explanation is these kidneys' relatively high kidney donor profile index (KDPI). Under KAS, kidney donors are classified into risk groups by KDPI, and pediatric transplant candidates receive allocation priority for kidneys with KDPI <35. Two factors in the KDPI, age and height, are formulated to confer the highest risk to young, small donors, meaning that their KDPI scores may be higher than their perceived risk. We sought to determine how the KDPI of small pediatric donor kidneys (<20 kg) aligns with graft survival and its potential impact on use.
Using SRTR standard analytic files, we examined the KDPI of small pediatric kidney donors and kidney graft survival in all KDPI ≥35 kidney-alone transplants January 1, 2010-September 30, 2016, stratified by KDPI group (35-85, ≥86) and donor size (≤20 kg, >20 kg).
All 2603 small donor kidneys recovered for transplant January 1, 2010-September 30, 2016 had KDPI >35: 44%, KDPI 35-85; 56% KDPI ≥86. However, among young pediatric (aged ≤10 years) candidates on the kidney waiting list December 4, 2014-September 30, 2016, 75% set their maximum acceptable KDPI to 85, and 7% to 35. Graft survival of small pediatric donor kidneys compared with larger donor kidneys by KDPI varied with time posttransplant (Figure 1). At 30 days posttransplant, graft survival was slightly worse for small-donor recipients than for their larger-donor counterparts (within KDPI). At 1 year, survival was comparables, and at 5 years, it was significantly better for small-donor recipients. Worse outcomes at 30 days likely reflected the more technically complex surgery that small donors require. However, we found no association between high small-donor transplant volume and improved outcomes.
KDPI may not accurately reflect the risk of small pediatric donor kidneys, and this may affect their use, particularly in pediatric candidates. Further study is needed of how best to quantify the risk of these small donor kidneys.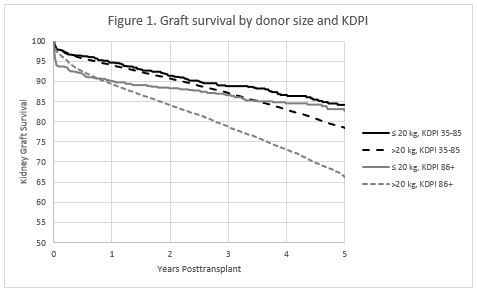
CITATION INFORMATION: Smith J, Gustafson S, Wey A, Snyder J, Israni A. KDPI and Small (<20 kg) Pediatric Kidney Donors. Am J Transplant. 2017;17 (suppl 3).
To cite this abstract in AMA style:
Smith J, Gustafson S, Wey A, Snyder J, Israni A. KDPI and Small (<20 kg) Pediatric Kidney Donors. [abstract]. Am J Transplant. 2017; 17 (suppl 3). https://atcmeetingabstracts.com/abstract/kdpi-and-small-20-kg-pediatric-kidney-donors/. Accessed March 1, 2026.« Back to 2017 American Transplant Congress
