Saftey & Long Term Outcomes of Tocilizumab (Anti-IL6R, TCZ) Therapy in Treatment of Chronic Antibody Mediated Rejection (CABMR) & Transplant Glomerulopathy (TG) in Highly-HLA Sensitized (HS) Patients (PTs).
1Comprehensive Transplant Center, Cedars-Sinai Medical Center, Los Angeles, CA
2Paris Transplant Group, University Paris Descartes, Paris, France
3Department of Pathology, Cedars-Sinai Medical Center, Los Angeles, CA
4Department of HLA Laboratory, Cedars-Sinai Medical Center, Los Angeles, CA
5Transplant Immunology Lab, Cedars-Sinai Medical Center, Los Angeles, CA
Meeting: 2017 American Transplant Congress
Abstract number: 289
Keywords: Antibodies, Immunosuppression, Kidney transplantation
Session Information
Session Name: Concurrent Session: Treatment of Antibody Mediated Rejection in Kidney Transplant Recipients
Session Type: Concurrent Session
Date: Monday, May 1, 2017
Session Time: 2:30pm-4:00pm
 Presentation Time: 2:30pm-2:42pm
Presentation Time: 2:30pm-2:42pm
Location: E354a
Introduction: DSAs in HS pts lead to poor allograft survival & return to a dialysis. Treatment options for CABMR and TG are limited. IL-6 appears to be important in mediating CABMR & TG. We report our experience with TCZ, (anti-IL6R), as a potential Rx for CABMR & TG. Methods: From 4/2011, we identified 52 CABMR+ pts with chronic TG & iDSA+. Pts received TCZ 4-8mg/kg monthly for 3-25 doses & followed up to 4Y. Pts were monitored for iDSA, renal function, pt/graft survival, AEs, & IgG levels. Results: Mean time from transplant to TCZ tx was 5.75±4.6 years. 44/52(85%) pts had significant pathologic findings of ABMR (34/52(65%) pts with TG). iDSA RIS were monitored up to 4Y post-TCZ . The majority of iDSAs were class II (DQs/DPs/DRs, 31/44(75%)) & 11/52 (21%) pts had C1Q+ iDSAs. After rx nonsignificant reductions in mean iDSA were seen (figure 1). SCr remained stable up to 4Y post TCZ initiation. Two deaths were noted unrelated to TCZ. Eight of 52 pts had hypogammglobulinemia of the 8 requiring monthly IVIG. Infectious and cardiovascular complications were minimal. Nine of 52 pts had repeat biopsies >1Y after initiation of TCZ, significant reductions were seen in C4d deposition (p = 0.0318) & glomerulo/peritubular capillaritis (p = 0.0175). Pt survival was 93.8% & graft survival was 80.5% at 6Y post-ABMR. Compared to CABMR +TG patients treated with SOC, TCZ treated pts had better graft outcomes (figure 2). Conclusions: With extended follow-up, CABMR & TG patients treated w/ TCZ continue to show long-term stabilization of renal function & graft survival in a population where much poorer outcomes would be expected.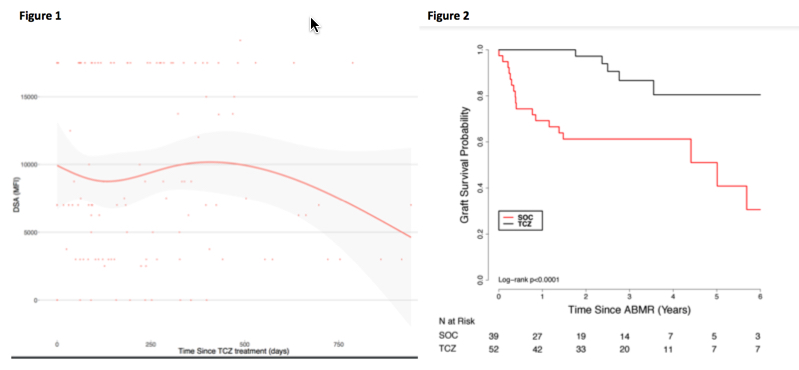
CITATION INFORMATION: Choi J, Aubert O, Vo A, Loupy A, Haas M, Louie S, Kang A, Peng A, Najjar R, Huang E, Toyota M, Zhang X, Jordan S. Saftey & Long Term Outcomes of Tocilizumab (Anti-IL6R, TCZ) Therapy in Treatment of Chronic Antibody Mediated Rejection (CABMR) & Transplant Glomerulopathy (TG) in Highly-HLA Sensitized (HS) Patients (PTs). Am J Transplant. 2017;17 (suppl 3).
To cite this abstract in AMA style:
Choi J, Aubert O, Vo A, Loupy A, Haas M, Louie S, Kang A, Peng A, Najjar R, Huang E, Toyota M, Zhang X, Jordan S. Saftey & Long Term Outcomes of Tocilizumab (Anti-IL6R, TCZ) Therapy in Treatment of Chronic Antibody Mediated Rejection (CABMR) & Transplant Glomerulopathy (TG) in Highly-HLA Sensitized (HS) Patients (PTs). [abstract]. Am J Transplant. 2017; 17 (suppl 3). https://atcmeetingabstracts.com/abstract/saftey-long-term-outcomes-of-tocilizumab-anti-il6r-tcz-therapy-in-treatment-of-chronic-antibody-mediated-rejection-cabmr-transplant-glomerulopathy-tg-in-highly-hla-sensitized-hs-p/. Accessed January 28, 2026.« Back to 2017 American Transplant Congress
