Long-Term Consequences of Post-Donation Preeclampsia.
1UofMN, Mpls
2M Health, Mpls
Meeting: 2017 American Transplant Congress
Abstract number: 259
Session Information
Session Name: Concurrent Session: Living Kidney Donation: Post Donation Issues
Session Type: Concurrent Session
Date: Monday, May 1, 2017
Session Time: 2:30pm-4:00pm
 Presentation Time: 3:30pm-3:42pm
Presentation Time: 3:30pm-3:42pm
Location: E450b
Preeclampsia (PE) has been linked to future development of ESRD in the general population. PE is more likely to occur in post-kidney donation pregnancies. Whether post-donation PE leads to ESRD in living donors (LD) is unknown and is unlikely to ever be ascertained considering that ESRD is a rare event after donation. We studied the association of PE with intermediate outcomes on the pathway to ESRD; namely, HTN, diabetes, proteinuria, and eGFR change over time.
From 1963 to 2013, our center performed 2360 LD nephrectomies from female LDs. These LDs were surveyed regarding any pregnancies and associated complications.
In total, 311 had a post-donation pregnancy of which 38 reported PE and 273 did not. LDs with PE were slightly younger at donation (23±4 vs 27±6, p<0.001) and a lower proportion had a pregnancy prior to donation (24% vs 54%, p<0.001) but were otherwise similar to LDs without PE.
After a mean follow-up of 25±12 years from donation and 21±12 years from the index post-donation pregnancy, 1 LD with PE developed ESRD from HTN vs. none in the LDs without PE. Additionally, 55% with vs 27% without developed HTN, 18% vs 7%, developed DM, and 18% vs 6% developed proteinuria.
In an analysis adjusted for characteristics at donation, LDs with PE were more likely to develop proteinuria and HTN, p<0.05 for each. We also examined the cumulative incidence of HTN and proteinuria after donation, with death considered to be a competing risk (Figure 1). LDs with PE had a significantly increased hazard for development of both conditions compared to those without PE (HR=2.72 and 4.16 respectively, p<0.05), Figure 1. Lastly, eGFR declined at -0.79 ml/min/year (95% CI -1.15, -0.43) in those with PE vs. -0.22 ml/min/year (95% CI -0.38, -0.07) in those without, p<0.01, Figure 2. Of note, these rates of eGFR decline are similar to what we have previously described in the general donor population, including males.
Conclusion: LDs with preeclampsia after donation are more likely to become proteinuric, hypertensive and their eGFR may decline at a faster rate. These outcomes are, however, comparable to what is seen in women with a history of PE and two kidneys and also male donors.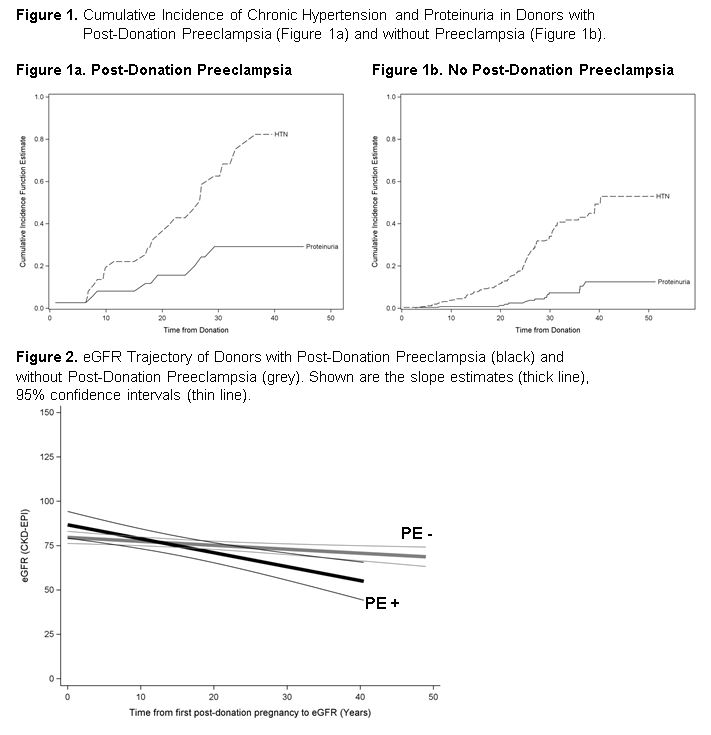
CITATION INFORMATION: Ibrahim H, Berglund D, Jackson S, Matas A. Long-Term Consequences of Post-Donation Preeclampsia. Am J Transplant. 2017;17 (suppl 3).
To cite this abstract in AMA style:
Ibrahim H, Berglund D, Jackson S, Matas A. Long-Term Consequences of Post-Donation Preeclampsia. [abstract]. Am J Transplant. 2017; 17 (suppl 3). https://atcmeetingabstracts.com/abstract/long-term-consequences-of-post-donation-preeclampsia/. Accessed January 16, 2026.« Back to 2017 American Transplant Congress
