A Retrospective Study to Describe the Epidemiology and Outcomes of Opportunistic Infections After Solid Organ Transplantation
1Northwestern University Transplant Research Collaborative, Chicago
2Infectious Diseases and Organ Transplantation, Northwestern University Feinberg SoM, Chicago.
Meeting: 2015 American Transplant Congress
Abstract number: C81
Session Information
Session Name: Poster Session C: Infections Risks/Prevention and Immunosuppression
Session Type: Poster Session
Date: Monday, May 4, 2015
Session Time: 5:30pm-6:30pm
 Presentation Time: 5:30pm-6:30pm
Presentation Time: 5:30pm-6:30pm
Location: Exhibit Hall E
Background: Solid organ transplant (SOT) recipients are at increased risk for infections due to their complex medical conditions and use of immunosuppressive therapies. Despite significant changes in induction and maintenance immunosuppression as well as infectious diseases prophylaxis, there is limited data on the contemporary epidemiology and outcomes of post-transplant infections.
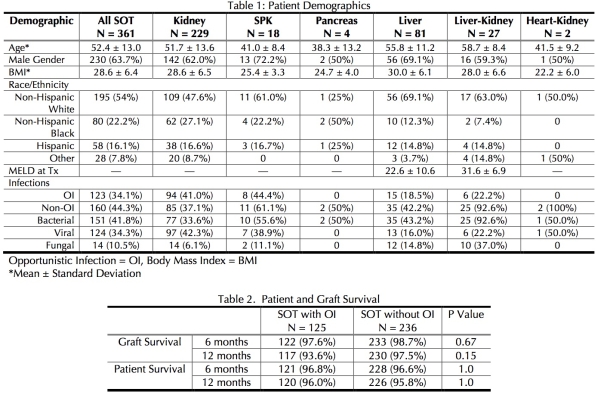
Methods: A retrospective chart review of all SOT recipients at Northwestern Memorial Hospital in 2012 was performed following IRB approval. Data collected included demographic and clinical variables including the type of transplant, indication for transplant, recipient mortality and morbidity, type of immunosuppression regimen, antimicrobial prophylaxis utilized, and documented infections. Patient and graft survival were assessed at 6 months and 1 year post-transplant. Fisher's exact test was utilized to compare survival rates.
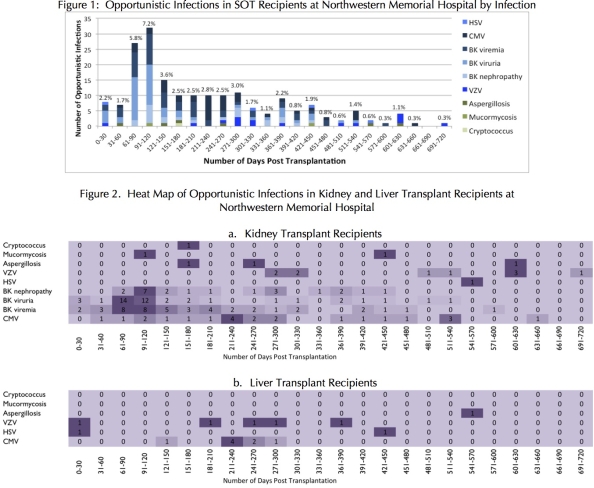
Results: Of the 361 SOT recipients, 123 (34.1%) had a documented opportunistic infection (OI) (detailed demographics, see Table 1). OIs were more common among kidney and SPK recipients; at NMH, only these patients received alemtuzumab. While OIs occur throughout the entire study period, the largest number of OIs occurred in months 3 (5.8%) and 4 (7.2%); rates remain high through month 10 (see figure 1). There was no difference in patient survival with a trend towards lower graft survival with OI at 12 months (Table 2).
Conclusions: Based on our data, the peak period of OI risk extends beyond the traditional 6 months and may require reassessment of risk mitigation strategies. Further analysis will attempt to define modifiable risk factors, including the use of alemtuzumab.
To cite this abstract in AMA style:
Helfrich M, Dorschner P, Ison M. A Retrospective Study to Describe the Epidemiology and Outcomes of Opportunistic Infections After Solid Organ Transplantation [abstract]. Am J Transplant. 2015; 15 (suppl 3). https://atcmeetingabstracts.com/abstract/a-retrospective-study-to-describe-the-epidemiology-and-outcomes-of-opportunistic-infections-after-solid-organ-transplantation/. Accessed February 17, 2026.« Back to 2015 American Transplant Congress
