Deceased Organ Donor Management: Does Hospital Volume Matter?
1Massachusetts General Hospital, Boston
2Portland Veterans Affairs Medical Center and Oregon Health & Science University, Portland.
Meeting: 2016 American Transplant Congress
Abstract number: 22
Keywords: Donation
Session Information
Session Name: Concurrent Session: Donor Management: All Organs
Session Type: Concurrent Session
Date: Sunday, June 12, 2016
Session Time: 2:30pm-4:00pm
 Presentation Time: 2:54pm-3:06pm
Presentation Time: 2:54pm-3:06pm
Location: Room 306
Purpose: Despite the association between hospital volume and outcomes for various diseases, there have been no studies to assess the impact of hospital organ donor volume on the number of organs transplanted per donor (OTPD).
Methods: A prospective observational study of all hospitals managing deceased organ donors covered by ten organ procurement organizations (OPOs) across UNOS Regions 4, 5, and 6 was conducted from February 2012-June 2015. Donor demographics, blood type, cause of death, OPO, and creatinine prior to procurement were collected prospectively through use of the UNOS Donor Management Goal Web Portal. In order to study the impact of hospital volume on organ yield, each donor was placed into a hospital volume quartile based on the number of donors managed by their hospital over the study period. Multivariate analysis was used to identify the independent effect of hospital volume on our primary outcome measure of having ≥ 4 OTPD.
Results: Data from 4427 donors across 384 hospitals were collected. Hospitals managed an average of 12±16 donors over the study period and were assigned quartiles based on their volume of deceased donors. Specifically, there were 97 hospitals in quartile 1 (lowest volume; managing an average of 1.4 ± 0.5 donors per hospital over the study period), 102 in quartile 2 (3.6 ± 1.7 donors), 89 in quartile 3 (9.2 ± 3.5 donors), and 96 in quartile 4 (highest volume; 32.3 ± 20.2 donors). After adjusting for age, ethnicity, donor type (standard criteria, expanded criteria, donor after circulatory determination of death), blood type, body mass index, creatinine, and OPO, being managed in hospitals within the highest volume quartile remained a positive independent predictor of ≥ 4 OTPD (OR 1.50 [1.28-1.77], P<0.001).
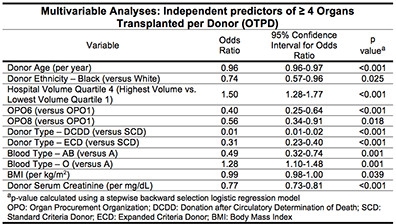
Conclusions: Deceased organ donor hospital volume impacts organ utilization rates, with the highest volume centers being 50% more likely to achieve ≥ 4 OTPD. Efforts should be made to share practices from these higher volume centers and consideration should be given to centralization of donor care.
CITATION INFORMATION: Patel M, Mohebali J, Sally M, Groat T, Vagefi P, Chang D, Malinoski D. Deceased Organ Donor Management: Does Hospital Volume Matter? Am J Transplant. 2016;16 (suppl 3).
To cite this abstract in AMA style:
Patel M, Mohebali J, Sally M, Groat T, Vagefi P, Chang D, Malinoski D. Deceased Organ Donor Management: Does Hospital Volume Matter? [abstract]. Am J Transplant. 2016; 16 (suppl 3). https://atcmeetingabstracts.com/abstract/deceased-organ-donor-management-does-hospital-volume-matter/. Accessed March 3, 2026.« Back to 2016 American Transplant Congress
