Evolution of Donor Nephrectomy: Long-Term Outcomes with Four Different Techniques Between 1963 and 2014 at a Single Institution.
O. Serrano,1 A. Bangdiwala,2 D. Vock,3 E. Minja,1 A. Pugalendhi,1 K. Yadav,1 V. Kirchner,1 W. Payne,1 T. Dunn,1 S. Chinnakotla,1 E. Finger,1 T. Pruett,1 A. Matas,1 R. Kandaswamy.1
1Surgery, Univ. of Minnesota, Minneapolis, MN
2Biostatistics and Bioinformatics Core, Masonic Cancer Center, Minneapolis, MN
3Biostatistics, Univ. of Minnesota, Minneapolis, MN.
Meeting: 2016 American Transplant Congress
Abstract number: C137
Keywords: Donation, Kidney transplantation, Living-related liver donors, Nephrectomy
Session Information
Session Name: Poster Session C: Kidney Donor Evaluation and Donor Nephrectomy
Session Type: Poster Session
Date: Monday, June 13, 2016
Session Time: 6:00pm-7:00pm
 Presentation Time: 6:00pm-7:00pm
Presentation Time: 6:00pm-7:00pm
Location: Halls C&D
PURPOSE: The development of minimally-invasive approaches to donor nephrectomy (DN) has been primarily driven by the potential advantages it presents the donor. Questions remain over the long-term outcomes of these newer techniques compared to traditional open DN.
METHODS: All donor and recipient records of DN performed between 1963 and 2014 were reviewed. Donor and recipient demographics, intraoperative parameters, complications, and short- and long-term outcomes were analyzed.
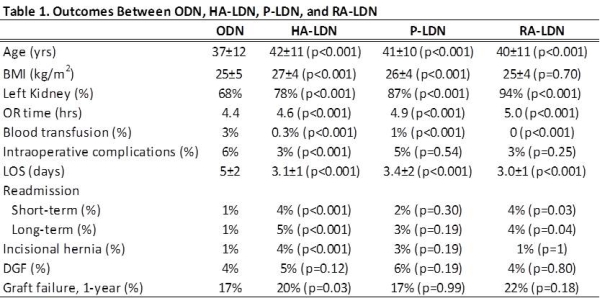
RESULTS: Between 1963 and 2014, we performed 4,296 DN: 2,638 open (ODN), 1,183 hand-assist laparoscopic DN (HA-LDN), 200 pure LDN (P-LDN), and 94 robotic-assist LDN (RA-LDN). Compared to ODN, LDN makes donation more accessible to an older and heavier (p<0.001) population. LDN has a higher probability of procuring the left kidney (p<0.001). All 3 modalities of LDN were found to require a longer operative time (p<0.001), with RA-LDN taking significantly longer than HA-LDN or P-LDN (p<0.001). LDN decreased the need for intraoperative blood transfusion (p<0.001), and reduced intraoperative complications (p<0.001) and hospital length of stay (p<0.001). However, short-term (p<0.001) and long-term (p<0.001) readmissions were significantly greater with LDN compared to ODN. HA-LDN was an independent risk factor for incisional hernia over all other modalities (p<0.001). Recipient delayed-graft was unaffected by surgical technique and 1-year graft failure seemed to be lower with LDN (p<0.001).
CONCLUSION: LDN has made kidney donation more accessible to a greater number of patients while decreasing intraoperative complications and hospital length of stay. These improvements in technique may be offset by a higher readmission rate and long-term complications.
CITATION INFORMATION: Serrano O, Bangdiwala A, Vock D, Minja E, Pugalendhi A, Yadav K, Kirchner V, Payne W, Dunn T, Chinnakotla S, Finger E, Pruett T, Matas A, Kandaswamy R. Evolution of Donor Nephrectomy: Long-Term Outcomes with Four Different Techniques Between 1963 and 2014 at a Single Institution. Am J Transplant. 2016;16 (suppl 3).
To cite this abstract in AMA style:
Serrano O, Bangdiwala A, Vock D, Minja E, Pugalendhi A, Yadav K, Kirchner V, Payne W, Dunn T, Chinnakotla S, Finger E, Pruett T, Matas A, Kandaswamy R. Evolution of Donor Nephrectomy: Long-Term Outcomes with Four Different Techniques Between 1963 and 2014 at a Single Institution. [abstract]. Am J Transplant. 2016; 16 (suppl 3). https://atcmeetingabstracts.com/abstract/evolution-of-donor-nephrectomy-long-term-outcomes-with-four-different-techniques-between-1963-and-2014-at-a-single-institution/. Accessed February 25, 2026.« Back to 2016 American Transplant Congress
