Acute-on-Chronic Liver Failure Admissions Cost 3 Times More Than Non-ACLF Related Admissions.
Baylor Simmons Transplant Institute, Baylor University Medical Center, Dallas, TX.
Meeting: 2016 American Transplant Congress
Abstract number: C66
Keywords: Economics, Infection, Liver cirrhosis, Liver failure
Session Information
Session Name: Poster Session C: Economics, Public Policy, Allocation, Ethics
Session Type: Poster Session
Date: Monday, June 13, 2016
Session Time: 6:00pm-7:00pm
 Presentation Time: 6:00pm-7:00pm
Presentation Time: 6:00pm-7:00pm
Location: Halls C&D
Background: Acute-on-chronic liver failure (ACLF) is associated with significant resource utilization. However, the relative charges associated with ACLF are not established.
Methods: We examined cirrhotics admitted to a tertiary care transplant center (February 2011-March 2015) who were prospectively enrolled in the North American Consortium for the Study of End-Stage Liver Disease (NACSELD). Cirrhotic patients non-electively admitted to the hospital in the absence of HIV, transplantation, or metastatic cancer were followed until 1-year post-discharge. ACLF, defined by NACSELD, is the presence of two or more organ failures including: circulatory (shock), brain (West Haven grade III/IV hepatic encephalopathy), renal (dialysis), and/or pulmonary (mechanical ventilation).
Results: 277 cirrhotic patients were included (mean (SD): 55 (9.3) years, 23% hepatitis C, Child score 10 (2.2), MELD score 20 (8.1)). Overall, 14% met ACLF criteria. Patients with ACLF had total mean charges 3 times greater than those without ACLF ($179,328 vs. $56,957 respectively, p<0.01) with longer lengths of stay (17 days vs. 8 days, p<0.01). The charges and LOS increased with the number of organ failures (0 organ failures: $52,372, 7.8 days, 1 organ failure: $94, 348, 11 days, 2 organ failures: $144,555, 15.8 days, and 3 organ failures: $230, 038, 18.2 days). Cirrhotics with 4 organ failures had lower charges ($122,435) related to early inpatient mortality. Cirrhotics with infection-related ACLF had total mean charges almost 3 times greater than non-infection related ACLF admissions ($161,556 vs. $57,501) and more than twice as high as infection related non-ACLF admissions ($68,621). In-hospital mortality in ACLF patients was 64% versus 3% for non-ACLF patients (p<0.01). While inpatient liver transplant rates were higher in patients with ACLF than without ACLF (8% vs. <1%, p=0.01), a similar number of patients with and without ACLF were transplanted within a year of discharge (2.5% vs 7%, p= 0.23).
Conclusion: Cirrhotics with ACLF-related admissions have significant resource utilization and increased LOS, especially when infections are present.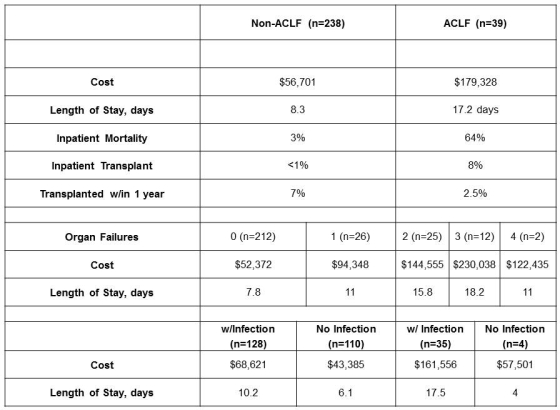
CITATION INFORMATION: Leffingwell S, O'Leary J, Asrani S. Acute-on-Chronic Liver Failure Admissions Cost 3 Times More Than Non-ACLF Related Admissions. Am J Transplant. 2016;16 (suppl 3).
To cite this abstract in AMA style:
Leffingwell S, O'Leary J, Asrani S. Acute-on-Chronic Liver Failure Admissions Cost 3 Times More Than Non-ACLF Related Admissions. [abstract]. Am J Transplant. 2016; 16 (suppl 3). https://atcmeetingabstracts.com/abstract/acute-on-chronic-liver-failure-admissions-cost-3-times-more-than-non-aclf-related-admissions/. Accessed February 19, 2026.« Back to 2016 American Transplant Congress
