Hospitalizations for Cardiovascular Disease After Kidney Transplantation: The Role of Facility Characteristics on Outcomes and Costs.
A. Mathur, Y.-H. Chang, D. Steidley, N. Katariya, A. Singer, W. Hewitt, K. Reddy, N. Wasif, D. Etzioni, A. Moss.
Mayo Clinic, Phoenix, AZ.
Meeting: 2016 American Transplant Congress
Abstract number: B234
Keywords: Economics, Kidney transplantation, Outcome, Post-operative complications
Session Information
Session Name: Poster Session B: Kidney: Cardiovascular and Metabolic
Session Type: Poster Session
Date: Sunday, June 12, 2016
Session Time: 6:00pm-7:00pm
 Presentation Time: 6:00pm-7:00pm
Presentation Time: 6:00pm-7:00pm
Location: Halls C&D
Background: Long term outcomes are in jeopardy when kidney transplant recipients are hospitalized with cardiovascular disease (CVD). We sought to understand hospital predictors of inpatient mortality and costs in this population.
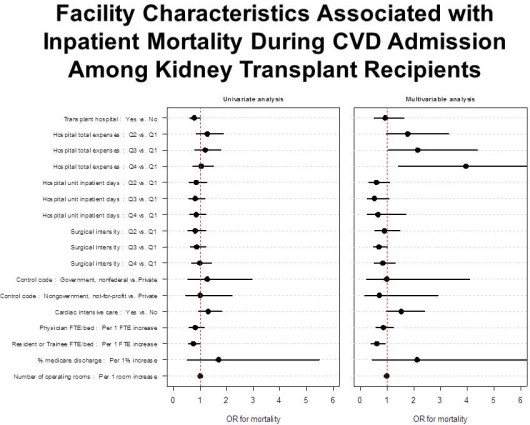
Methods: We merged data from the 2009-2011 Nationwide Inpatient Sample and the American Hospital Association Survey to evaluate kidney transplant patients hospitalized for MI, CHF, stroke, cardiac arrest, dysrhythmia, and malignant hypertension. Cost data were abstracted using standardized cost-to-charge ratios. We used generalized estimating equations to study the effect of facility characteristics on risk-adjusted mortality and costs.
Results: 7,803 hospital admissions were evaluated from 275 hospitals. 29.4% of facilities did not have transplant programs (n=78). Median overall hospital-specific mortality was 3.4% (IQR 0-5.9%). Age, CVD burden, need for dialysis, and inpatient transfer predicted mortality (all, p<0.001). Facility characteristics associated with risk-adjusted mortality included higher total expenses, cardiac intensive care, fewer trainees, CVD destination status (all, p<0.05), regardless of patient dialysis. Transplant hospital status was not associated with risk-adjusted mortality (aOR 0.97, p=0.91).
Transplant centers had significantly higher un-adjusted total charges (Median $33,271 vs $28,022 per episode, p<0.0001). MI, stroke, dysrhythmia, and cardiac arrest were associated with significantly higher costs vs. CHF (all, p<0.001). Hospital factors associated with higher costs were CVD destination status (aOR 1.24, p<0.001), hospital size (p<0.05), and greater physician density (aOR 1.13, p=0.01). Cardiac specialty services, but not transplant services, were associated with higher costs (all, p<0.05).
Conclusions: Hospital characteristics are significantly associated with mortality and costs in CVD treatment after transplant, independent of patient factors. Further study of CVD care processes by transplant programs are warranted to improve outcomes and cost savings.
CITATION INFORMATION: Mathur A, Chang Y.-H, Steidley D, Katariya N, Singer A, Hewitt W, Reddy K, Wasif N, Etzioni D, Moss A. Hospitalizations for Cardiovascular Disease After Kidney Transplantation: The Role of Facility Characteristics on Outcomes and Costs. Am J Transplant. 2016;16 (suppl 3).
To cite this abstract in AMA style:
Mathur A, Chang Y-H, Steidley D, Katariya N, Singer A, Hewitt W, Reddy K, Wasif N, Etzioni D, Moss A. Hospitalizations for Cardiovascular Disease After Kidney Transplantation: The Role of Facility Characteristics on Outcomes and Costs. [abstract]. Am J Transplant. 2016; 16 (suppl 3). https://atcmeetingabstracts.com/abstract/hospitalizations-for-cardiovascular-disease-after-kidney-transplantation-the-role-of-facility-characteristics-on-outcomes-and-costs/. Accessed March 3, 2026.« Back to 2016 American Transplant Congress
